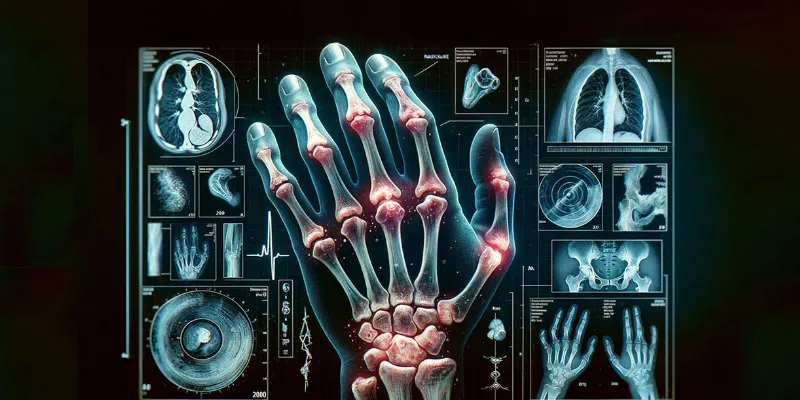
New Cellular Atlas Promises Personalized Medicine in Rheumatoid Arthritis Treatment
11 November 2023
A new study, published in Nature, has identified six distinct inflammation types in rheumatoid arthritis, each with unique cellular characteristics. Researchers analyzed over 314,000 cells from affected tissues, revealing diverse disease pathways. This significant finding, paving the way for more precise, tailored treatments, represents a major step towards personalized medicine in combating this autoimmune disease.
Researchers have charted new territory in the fight against rheumatoid arthritis (RA), a debilitating autoimmune disease affecting approximately 18 million people worldwide. This innovative research, a collaborative effort led by the Broad Institute of MIT and Harvard along with Brigham and Women's Hospital, offers hope for more personalized and effective treatments for RA sufferers.
Rheumatoid arthritis, characterized by painful inflammation leading to joint damage and disability, has long presented a challenge to medical professionals. Despite the development of therapies targeting specific inflammatory pathways, many patients still struggle with persistent symptoms.
The research team took an unprecedented approach, analyzing over 314,000 cells from RA tissue to unravel the disease at a single-cell level.
This comprehensive analysis led to the identification of six distinct inflammation types in RA, each involving different cell types and disease pathways.
These subtypes, termed cell-type abundance phenotypes (CTAPs), range from those enriched in T and B cells to those surprisingly dominated by structural cells like fibroblasts and endothelial cells, with fewer inflammatory leukocytes.
Dr. Soumya Raychaudhuri, MD, PhD, from Brigham’s DR and study's corresponding author, emphasized the importance of this research in understanding why some RA patients do not respond to conventional treatments:
“In the treatment of individuals with rheumatoid arthritis, we struggle to find the right treatment for the right patient. We aimed to determine why some subsets of patients don’t respond to conventional treatments by looking at the subtypes of inflammation. We did so from many different angles, using multiple cutting-edge, single-cell techniques and integrating results in a way that hasn’t been done before for an inflammatory disease.”
The findings highlight the dynamic nature of CTAPs in patients, which can evolve in response to treatment. This discovery opens new avenues for patient-specific therapy approaches.
Dr. Michael Brenner, another senior researcher on the team, underscored the significance of synovial tissue analysis in RA patients, a practice not currently standard:
“Our findings point to the value of getting synovial tissue biopsies to evaluate the nature of the pathological process, which can be so different across patients. Clinical trials going forward will benefit greatly from assessing tissue characteristics alongside responses to a therapy. By providing this atlas of cell types and pathways involved in RA, we are better able to pursue our precision medicine goal of being able to select the right drug for the right patient and achieve a high response rate.”
The implications of this study are far-reaching, promising a new era in the treatment of rheumatoid arthritis. By mapping the cellular landscape of RA, researchers have provided a crucial atlas to guide future therapeutic strategies, offering hope to millions afflicted by this chronic condition.
Abstract of the research
Deconstruction of rheumatoid arthritis synovium defines inflammatory subtypes
Abstract: Rheumatoid arthritis is a prototypical autoimmune disease that causes joint inflammation and destruction1. There is currently no cure for rheumatoid arthritis, and the effectiveness of treatments varies across patients, suggesting an undefined pathogenic diversity1,2. Here, to deconstruct the cell states and pathways that characterize this pathogenic heterogeneity, we profiled the full spectrum of cells in inflamed synovium from patients with rheumatoid arthritis. We used multi-modal single-cell RNA-sequencing and surface protein data coupled with histology of synovial tissue from 79 donors to build single-cell atlas of rheumatoid arthritis synovial tissue that includes more than 314,000 cells. We stratified tissues into six groups, referred to as cell-type abundance phenotypes (CTAPs), each characterized by selectively enriched cell states. These CTAPs demonstrate the diversity of synovial inflammation in rheumatoid arthritis, ranging from samples enriched for T and B cells to those largely lacking lymphocytes. Disease-relevant cell states, cytokines, risk genes, histology and serology metrics are associated with particular CTAPs. CTAPs are dynamic and can predict treatment response, highlighting the clinical utility of classifying rheumatoid arthritis synovial phenotypes. This comprehensive atlas and molecular, tissue-based stratification of rheumatoid arthritis synovial tissue reveal new insights into rheumatoid arthritis pathology and heterogeneity that could inform novel targeted treatments.


Comments
No Comments Yet!