Novel Biomarker-Driven Treatments with ADCs in NSC Lung Cancer Management

ONCOLife |
5 November 2024
Antibody-drug conjugates (ADCs) represent a significant breakthrough in oncology, offering targeted treatments, especially for lung cancer. In this insightful interview with Dr. Nicolas Girard, Head of the Curie-Montsouris Thorax Institute and Professor of Respiratory Medicine, we explore the evolving role of ADCs in treating non-small cell lung cancer (NSCLC).
Professor Girard discusses the results of the LUMINOSITY Phase 2 trial, which demonstrated significant improvements in progression-free survival and overall survival in patients with NSCLC. Dr. Girard’s work has been at the forefront of this cutting edge research, and he highlights the importance of biomarker-driven patient stratification and the future potential of combining ADCs with chemotherapy and immune checkpoint inhibitors.
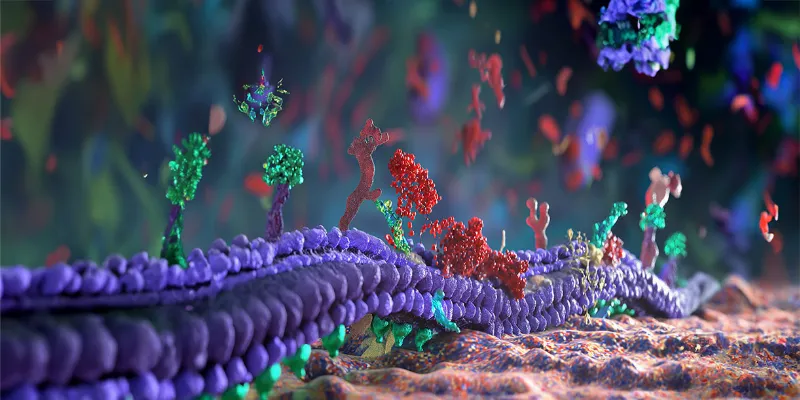
Click the picture to view the PDF version: Pg 6-9.
How does your research at Institut Curie integrate precision medicine principles, particularly in targeting overexpressed protein biomarkers in solid tumors?
Dr. Girard: We are shifting from focusing on molecular alterations, such as activating mutations and gene fusions, to a different approach that involves identifying novel biomarkers to facilitate the entry of cytotoxic agents via antibodies.
This approach to biomarkers is different, shifting from next-generation sequencing based DNA/RNA alterations to a more functional view which focuses on the expression of targets on the surface of cancer cells and requires different techniques, such as immunohistochemistry. Of note, this expression may change over time due to disease progression and exposure to anticancer agents. Thus, targets can evolve from initial diagnosis to more advanced stages.
Could you elaborate on the potential of ADCs like Telisotuzumab Vedotin in overcoming the challenges of treating solid tumors such as lung cancer?
Dr. Girard: Telisotuzumab vedotin (Teliso-V) is an investigational ADC targeting c-Met protein. C-Met is an oncogene found to be overexpressed on the surface of cancer cells in lung cancer and other solid tumors. Teliso-V has demonstrated antitumor efficacy in the LUMINOSITY Phase 2 study, particularly in patients with advanced, refractory NSCLC after failure of first-line chemotherapy and immunotherapy.
In this study, the highest efficacy was seen in patients with non-squamous cell carcinoma and overexpression of c-Met, without other oncogene alterations. In c-Met intermediate and high patients, the response rates were 23 and 35%, respectively, showing a clear correlation between efficacy and the level of c-Met expression.
At ESMO this year, we presented exploratory PRO analyses from the LUMINOSITY study, which showed patterns of improvement in key lung cancer symptoms, and maintenance of QoL and physical functioning over time. Now, we have a Phase 3 trial, TeliMET study evaluating Teliso-V as a monotherapy, compared to docetaxel, in patients with previously treated c-Met overexpressing EGFR wild type non-squamous NSCLC.
As discussed earlier, it’s important to assess c-Met expression before starting the trial, and prebiopsy may be necessary if c-Met is negative at the time of initial diagnosis as it could become positive after previous chemotherapy or immunotherapy. This ensures we capture the full benefits of Teliso-V in terms of survival outcomes.
What are the key takeaways from the Phase 2 LUMINOSITY trial regarding the efficacy and safety of Teliso-V in patients with c-Met overexpressing, EGFR wildtype NSCLC?
Dr. Girard: As I described, the overall response rate is 30%, which is higher than that of docetaxel, which usually maxes out at 15%. This response rate provides a strong rationale to move to Phase 3 trials. We observed median duration of response per ICR of 9 months and 7.2 months and a median overall survival of 14.6 months and 14.2 months across c-Met High and c-Met Intermediate patients respectively.
Additionally, patient-reported outcomes (PROs) from the LUMINOSITY study were very interesting. There was prolonged time to deterioration in quality of life and symptoms, in patients who responded to treatment including in those with stable disease. This shows that even stable disease in this advanced refractory setting significantly improves patients’ quality of life. We also saw improvements in key symptoms like cough and chest pain.
Regarding the safety of Teliso-V, as an ADC, its side effects are linked to MET inhibition, such as edema, though rare, and to the cytotoxic payload, which can cause peripheral neuropathy - a known cumulative toxicity associated with ADCs using the monomethyl auristatin E (MMAE) payload.
This neuropathy tends to occur in long-term responders, and while Grade 3-4 neuropathy is rare, it is manageable with preventive measures. ADC side effects differ from those seen with traditional chemotherapy, and we must take a multidisciplinary approach to effectively manage the associated toxicities.
Additionally, ADCs may co-me with other side effects, including interstitial lung disease (ILD), stomatitis, ocular toxicities, and hematological issues. At Institut Curie, we established an ADC clinic where specialists work together to manage these side effects proactively.
We don’t wait for side effects to worsen before acting. This multidisciplinary approach, similar to how we adapted to immune checkpoint inhibitors, is crucial for effectively managing ADC-related toxicities.
Can you discuss the significance of PROs in the LUMINOSITY trial, particularly in assessing quality of life and symptom management in lung cancer patients treated with Teliso-V?
Dr. Girard: So, as I mentioned, PROs are very important, especially in Phase 2 studies, to understand what is meaningful for patients. With this drug’s new mechanism of action, we need to determine if the reported side effects truly impact quality of life and to what extent.
Additionally, we must explore the relationship between response and the actual benefit for the patient. Including PROs in the assessment of new agents, particularly in Phase 2 trials, adds value not only for healthcare authorities but also for clinicians and patients.
Are there any plans to explore Teliso-V in combination with other therapies, such as immune checkpoint inhibitors or targeted therapies, to enhance treatment efficacy in lung cancer?
Dr. Girard: We’re not quite there yet with Teliso-V but ADCs may be combined with immune checkpoint inhibitors, and there are many ongoing trials with TROP2 inhibitors like datopotamab deruxtecan. We know this combination is safe, without an increase in side effects or any synergistic toxicity.
It’s a great opportunity in lung cancer to move from late-line to first-line treatment, where the standard of care involves immune checkpoint inhibitors. The key question is how to select the right patient population in terms of biomarkers, not only for immune therapy with PD-L1 expression but also for the ADC.
What are the next steps in your research on ADCs and precision medicine? Are there any upcoming trials or novel targets that you are particularly excited about?
Dr. Girard: There are many potential novel targets, and the key question is whether these targets are co-expressed or not. If we have a panel of targets and ADCs, what will the treatment sequence be? Which target should be prioritized? It likely comes down to quantification, and using QCS and digitalization of immunohistochemistry slides is a promising approach. Unlike mutually exclusive molecu-lar alterations, we are dealing with multiple biomarkers that may be co-expressed.
How do you envision the role of ADCs evolving in the broader landscape of oncology treatment? What breakthroughs do you anticipate in the next 5-10 years that could significantly alter patient outcomes?
Dr. Girard: We are moving toward combining ADCs with chemotherapy and immune checkpoint inhibitors. The key question is: who benefits from this escalation? We need better patient stratification to determine who truly requires this intensification and who may not benefit from these combinations.











Comments
No Comments Yet!