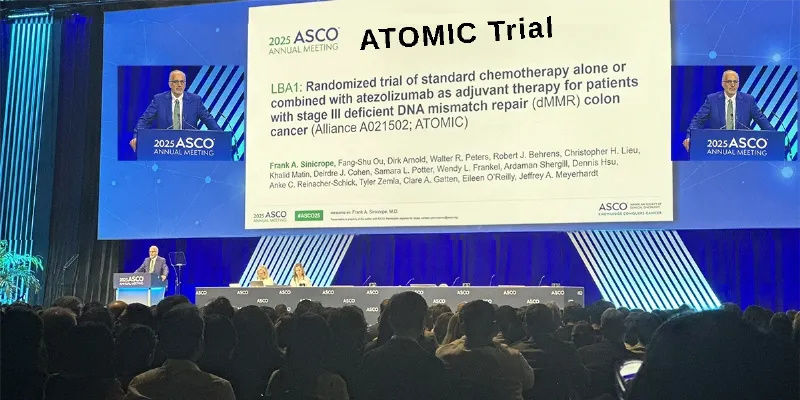
ATOMIC Trial: Atezolizumab Combo Halves Recurrence in Stage III dMMR Colon Cancer
3 June 2025
Atezolizumab (Tecentriq) plus FOLFOX chemotherapy halved the risk of recurrence or death in stage III dMMR colon cancer, boosting three-year disease-free survival (DFS) to 86.4% versus 76.6% with chemotherapy alone, according to the ATOMIC trial. Presented at ASCO 2025, these results position chemoimmunotherapy as a potential new standard of care for this subgroup.
The new data from the randomized phase 3 ATOMIC trial were presented at the 2025 American Society of Clinical Oncology (ASCO) Annual Meeting, marking a milestone in the treatment landscape for colorectal cancer. This multicenter trial demonstrated that adding the immune checkpoint inhibitor atezolizumab to standard adjuvant chemotherapy significantly reduced the risk of recurrence and death in patients with stage III colon cancer harboring deficient DNA mismatch repair (dMMR).
“Our study demonstrates that the addition of immunotherapy—the anti–PD-L1 antibody atezolizumab—to FOLFOX chemotherapy can significantly improve DFS compared to FOLFOX alone in patients with stage III, lymph node–positive colon cancers with dMMR,” said Dr. Frank A. Sinicrope of the Mayo Clinic in Rochester, who presented the trial during the Plenary Session. He pointed out that the results will most likely lead to chemoimmunotherapy becoming a standard of care for these patients.
Key Findings from the ATOMIC Trial
The ATOMIC trial enrolled 712 patients with resected stage III dMMR colon cancer across multiple centers from 2017 to 2023. Patients were randomized to receive either standard FOLFOX chemotherapy or FOLFOX plus atezolizumab for six months, followed by an additional six months of atezolizumab alone.
Dr. Sinicrope showed a striking 50% reduction in the risk of disease recurrence or death in the combination arm compared with chemotherapy alone (hazard ratio 0.50; 95% CI, 0.34–0.72; P < .0001). At three years, the disease-free survival (DFS) rate reached 86.4% in the atezolizumab arm versus 76.6% in the chemotherapy-alone group—a robust and clinically meaningful improvement.
Importantly, the DFS benefit was consistent across diverse subgroups, including age, sex, race, tumor location, and disease stage, underscoring the broad applicability of this strategy in the dMMR patient population. Overall survival data are not yet mature, with a median follow-up of 42.5 months, and future analyses will need to account for subsequent treatments with immunotherapy.
Dr. Myriam Chalabi, from the Netherlands Cancer Institute, noted during the ASCO Plenary Session that this is the first study to provide data on adjuvant immunotherapy in patients with dMMR stage III colon cancer. Dr. Chalabi added that “it’s a positive study,” and, if approved, the combination of atezolizumab plus FOLFOX will add “to the arsenal of treatments that we can give patients with dMMR colon cancers.”
Safety Profile and Considerations
The addition of atezolizumab was associated with a higher incidence of grade 3 or greater adverse events compared to chemotherapy alone. Common toxicities included fatigue, nausea, anorexia, and laboratory abnormalities such as decreased white blood cell and neutrophil counts, as well as elevated aspartate aminotransferase. Notably, the rates of grade 4 neutropenia were 14.0% in the combination arm versus 7.0% in the chemotherapy-alone arm.
Despite these side effects, the trial did not reveal significant differences in severe immune-related adverse events, providing reassurance about the safety of adding atezolizumab in this setting.
Implications for Clinical Practice and Future Directions
These findings establish a new standard of care for patients with resected stage III dMMR colon cancer, extending the role of immunotherapy beyond the metastatic setting.
Dr. Sinicrope emphasized that the results are particularly relevant for patients with Lynch syndrome—the most common hereditary colorectal cancer syndrome—and for sporadic dMMR tumors, offering new hope for improved long-term outcomes.
A New Chapter in dMMR Colon Cancer
Stage III colon cancer, typically treated with adjuvant chemotherapy regimens such as FOLFOX (5-fluorouracil, leucovorin, and oxaliplatin), remains a significant clinical challenge, particularly in younger patients, whose disease often presents at more advanced stages.
Approximately 10% to 15% of nonmetastatic colorectal cancers globally are characterized by dMMR, a feature conferring resistance to fluoropyrimidine-based chemotherapy and linked to high microsatellite instability (MSI). While immunotherapy has proven effective in metastatic dMMR tumors, its role in the adjuvant setting had been unclear—until now.











Comments
No Comments Yet!