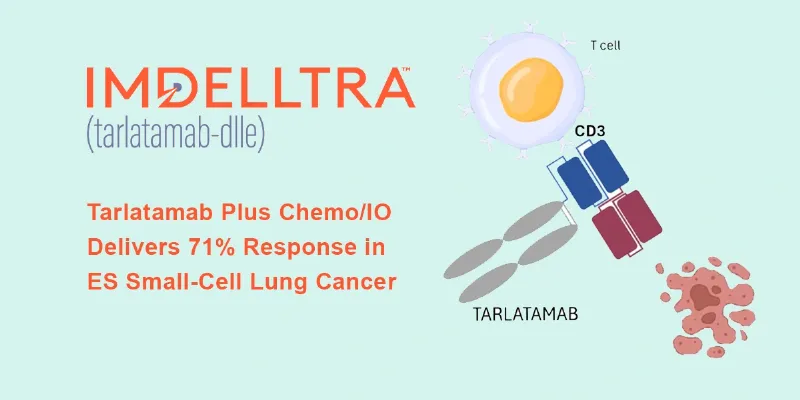
DeLLphi-303: Tarlatamab Plus Chemo Achieves 71% Response in ES Small-Cell Lung Cancer
4 November 2025
New data from the phase 1b DeLLphi-303 study presented at ESMO 2025 Congress show that adding the DLL3-targeted bispecific T-cell engager tarlatamab to first-line chemoimmunotherapy achieved a 71% response rate and 10.3-month median PFS in extensive-stage small-cell lung cancer (ES-SCLC), with manageable cytokine-related toxicity and a median overall survival of 25.3 months in the maintenance cohort.
At this year’s ESMO 2025 Congress in Berlin, investigators presented encouraging results from the phase 1b DeLLphi-303 study (NCT05361395), evaluating tarlatamab (Imdelltra) in combination with platinum–etoposide and a PD-L1 inhibitor in the frontline setting, followed by maintenance therapy with tarlatamab and PD-L1 blockade. Tarlatamab is a delta-like ligand 3 (DLL3)-directed bispecific T-cell engager (BiTE) that redirects T cells to attack DLL3-expressing SCLC cells, a target expressed on more than 80% of tumors but absent in healthy lung tissue.
Promising Efficacy Across Early Data
Among 96 patients with ES-SCLC, the combination of tarlatamab plus chemoimmunotherapy achieved an objective response rate (ORR) of 71%, with complete responses in 5% and partial responses in 66% of patients. Another 11% maintained stable disease, while 8% had progression at data cutoff.
Responses were durable, with a median duration of response (DOR) of 11 months, a median progression-free survival (PFS) of 10.3 months, and 12-month PFS and overall survival (OS) rates of 43% and 81%, respectively. Nearly half of patients (49%) continued to respond at the time of data analysis.
Maintenance Therapy Reinforces Long-Term Benefit
An additional cohort of 88 patients received tarlatamab with atezolizumab or durvalumab as first-line maintenance therapy following chemoimmunotherapy. At a median follow-up of 18.4 months, the median overall survival reached 25.3 months, with no treatment-related deaths reported.
The most frequent grade 3–4 adverse events included hyponatremia (10%), anemia (8%), and neutropenia (7%). Cytokine release syndrome (CRS) occurred in 24% and immune effector cell–associated neurotoxicity syndrome (ICANS) in 5% of patients, mostly low-grade and reversible.
Toward Biomarker-Guided Therapy in SCLC
Unlike non-small-cell lung cancer, SCLC lacks validated biomarkers to guide therapy. DLL3, overexpressed on most SCLC cells, may represent a path toward molecularly targeted treatment in this historically homogeneous disease.
“Although CRS and ICANS are potential concerns, the low incidence of severe events indicates that, in experienced hands and with well-selected patients, this approach is feasible,” notes Prof. Suresh Senan from Amsterdam University Medical Centers, Netherlands.
Tarlatamab also represents a step toward biomarker-guided therapy, explains Senan. “The extensive cell expression of the tarlatamab target is about as close as we currently have to a biomarker in ES-SCLC. Future translational studies will be critical to identify patients who may benefit most from its early use.”
A Manageable Safety Profile
In the frontline combination arm, nearly all patients experienced treatment-related adverse events, though only 6% discontinued tarlatamab due to toxicity. Grade 3 or 4 events occurred in 78% of patients, most often hematologic, reflecting the chemotherapy component. CRS and ICANS were largely mild, emerging mainly during the first treatment cycle, and all cases resolved with standard supportive care. Importantly, no additive or synergistic toxicity was observed between tarlatamab and PD-L1 inhibitors.











Comments
No Comments Yet!