Trodelvy Emerges as Potential New Standard for First-Line Metastatic TN Breast Cancer
24 October 2025
Findings from the Phase 3 ASCENT-03 trial, demonstrated that sacituzumab govitecan (Trodelvy®) significantly reduced the risk of disease progression or death by 38% compared with chemotherapy in untreated metastatic triple-negative breast cancer (TNBC) patients ineligible for PD-1/PD-L1 inhibitors. Median progression-free survival was 9.7 versus 6.9 months, establishing Trodelvy as a potential new first-line standard for this hard-to-treat population.
Results from the international Phase 3 ASCENT-03 trial show that the antibody–drug conjugate (ADC) sacituzumab govitecan (Trodelvy) significantly prolonged progression-free survival (PFS) in first-line mTNBC. Presented as a late-breaking abstract at the 2025 ESMO Congress and published simultaneously in the NEJM, the study demonstrated a 38% reduction in the risk of disease progression or death with Trodelvy compared with chemotherapy.
The PFS results for Trodelvy versus chemotherapy were consistent across prespecified subgroups, including among patients with poorer prognosis and regardless of chemotherapy chosen.
“Patients with metastatic TNBC who are ineligible for immunotherapy face an especially poor prognosis, with limited treatment options and fast disease progression,” said Dr. Javier Cortés, Head of the International Breast Cancer Center in Spain and principal investigator of the ASCENT-03 study.
“The ability of sacituzumab govitecan to significantly delay death and progression could represent the first major treatment advance for this patient population in the 20 years since TNBC was defined, marking an historic shift and establishing a potential new standard of care.”
Study Overview
ASCENT-03 was a global, open-label, randomized trial enrolling 558 patients with previously untreated, locally advanced, inoperable, or metastatic TNBC who were ineligible for PD-1/PD-L1 blockade—either due to PD-L1–negative disease (combined positive score <10) or prior exposure to PD-(L)1 inhibitors in the curative setting.
Patients were randomized 1:1 to receive sacituzumab govitecan or physician’s choice of chemotherapy, which included paclitaxel, nab-paclitaxel, or gemcitabine plus carboplatin. Treatment continued until disease progression or unacceptable toxicity. The primary endpoint was progression-free survival assessed by blinded independent central review (BICR). Secondary endpoints included overall survival (OS), objective response rate (ORR), duration of response (DOR), and safety.
Key Efficacy Findings
The benefit of sacituzumab govitecan was consistent across prespecified subgroups, including those with early recurrence following prior therapy.
- Median PFS: 9.7 vs. 6.9 months (HR, 0.62; P<0.001)
- Objective Response Rate: 48% (95% CI, 42–54) with sacituzumab govitecan vs. 46% (95% CI, 40–52) with chemotherapy
- Median Duration of Response: 12.2 vs. 7.2 months
Although overall survival data remain immature, follow-up is ongoing. The magnitude and consistency of the PFS benefit suggest potential for clinically meaningful OS improvement, pending future analyses.
Safety and Tolerability
The safety profile of sacituzumab govitecan was in line with previous studies, with no new safety signals identified. Grade ≥3 treatment-emergent adverse events (TEAEs) occurred in 66% of patients in the ADC arm and 62% in the chemotherapy arm. The most common grade ≥3 toxicities were:
- Neutropenia: 43% (Trodelvy) vs. 41% (chemotherapy)
- Diarrhea: 9% (Trodelvy) vs. 3% (chemotherapy)
- Leukopenia: 7% (Trodelvy) vs 13% (chemo)
- Anemia: 4% (Trodelvy) vs. 16% (chemotherapy)
Importantly, treatment discontinuations due to adverse events were less frequent with sacituzumab govitecan (4%) than with chemotherapy (12%), suggesting favorable manageability.
“ASCENT-03 is the second Phase 3 trial with a Trodelvy-based regimen to show superior progression-free survival over chemotherapy in first-line metastatic TNBC, highlighting its potential to improve outcomes for patients with limited treatment options,” said Dr. Dietmar Berger, Chief Medical Officer, Gilead Sciences. “With these potentially practice-changing results, Trodelvy is poised to transform the first-line metastatic TNBC treatment landscape, offering a much-needed alternative to chemotherapy.”
Clinical and Regulatory Implications
The ASCENT-03 findings complement results from ASCENT-04/KEYNOTE-D19, in which sacituzumab govitecan combined with pembrolizumab improved PFS in PD-L1–positive first-line metastatic TNBC. Together, the two Phase 3 studies position Trodelvy as the first antibody-drug conjugate to demonstrate superiority over chemotherapy in both PD-L1–positive and PD-L1–negative first-line TNBC. Gilead is engaging with the U.S. FDA and other global regulators regarding both data sets.
About Trodelvy:
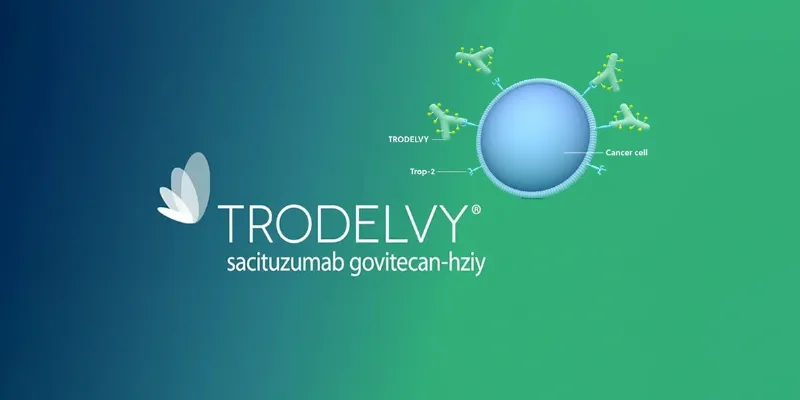
Trodelvy® (sacituzumab govitecan-hziy) is a first-in-class Trop-2–directed antibody-drug conjugate (ADC) that links a monoclonal antibody to SN-38, a topoisomerase I inhibitor, via a hydrolyzable linker. By targeting Trop-2, expressed in over 90% of breast and lung cancers, Trodelvy delivers cytotoxic activity to tumor cells and their microenvironment through a bystander effect. It is approved in more than 50 countries for second-line or later metastatic TNBC and in over 40 for pretreated HR+/HER2– disease. Multiple Phase 3 trials are evaluating Trodelvy across Trop-2–expressing solid tumors and earlier treatment settings.











Comments
No Comments Yet!