Dr. Johan Baeck Discusses PT-112: A New Frontier in Immuno-Oncology
15 February 2024
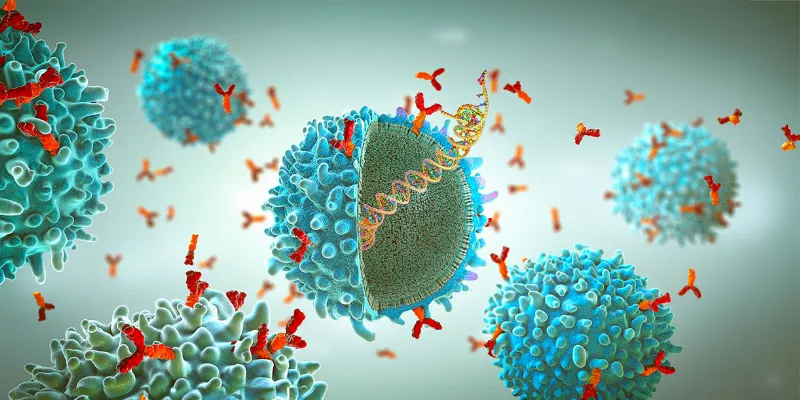
In an exclusive interview with ONCOLife, Dr. Johan Baeck, Chief Medical Officer at Promontory Therapeutics, discusses PT-112, a groundbreaking cancer therapy targeting ribosomal biogenesis, marking a shift in immuno-oncology. Dr. Baeck highlights PT-112’s unique ability to effectively target tumors while preserving healthy cells, engaging immune responses, and showing promise in treating ‘immune cold’ cancers.
Shifting Paradigms in Oncology and the Promise of PT-112
Can you elaborate on the unique mechanism of action of PT-112, particularly its ability to inhibit ribosomal biogenesis and how this contributes to its anti-cancer immune response?
Dr. Johan Baeck: In our innovative approach with PT-112, we’ve shifted focus from targeting nuclear DNA to inhibiting ribosomal biogenesis in cancer cells. This method is particularly compelling because it’s well tolerated by healthy cells, a crucial aspect of our drug’s safety profile. Cancer cells, driven by their inherent need to proliferate, require substantial protein production, hence a greater number of ribosomes.
Click the picture to view the PDF version: Pg 24-28.
PT-112 uniquely targets this proliferation by hindering ribosomal biogenesis specifically in cancer cells, sparing healthy ones. This selective inhibition not only demonstrates efficacy in tumor reduction but also ensures safety. Furthermore, PT-112 induces stress in cancer cell organelles, leading to an integrated stress response. This contributes to the drug’s immunogenic effects, highlighting PT-112’s potential as a targeted and innovative treatment in oncology.
The concept of immunogenic cell death is central to PT-112’s strategy. How does PT-112’s induction of ICD differ or improve upon existing immunotherapies in oncology?
Dr. Johan Baeck: Checkpoint inhibitors like pembrolizumab act by directly interacting with and activating T-cells. While this has proven to be an effective approach for many diseases, these drugs have a limited ability to recruit T-cell to the cancer in the context of immune cold disease. PT-112 acts directly on cancer cells and can stimulate the recruitment of immune cells to the tumor micro environment.
Because this approach is very different from that of checkpoint inhibitors, this means PT-112 both can work in areas where checkpoints work poorly, and can be used in conjunction with checkpoints in a synergistic fashion. This underscores PT-112’s potential to fill a significant gap in treatment options for cancers with inactive or insufficient T-cell presence.
PT-112 has shown an ability to engage both adaptive and innate immune responses. Could you discuss the significance of this dual engagement for cancer treatment?
Dr. Johan Baeck: The immune system comprises two key components: the innate system, which acts immediately against foreign threats, and the adaptive system, known for its precision and ability to provide long-term benefits through memory. Our research, in collaboration with the National Cancer Institute, has yielded independent validation of PT-112, positively impacting both the innate and adaptive immune responses.
These findings have been presented at prestigious medical conferences, including ASCO 2023 and the International Thymic Malignancy Interest Group (ITMIG). A significant breakthrough was demonstrating PT-112’s capability to engage with both immune system components in the bloodstream and within the tumor’s microenvironment.
Additionally, recent studies highlight the potential of natural killer cells, part of the innate system, being activated through immunogenic cell death. This suggests PT-112 could serve as a pivotal bridge between the innate and adaptive systems, enhancing the overall immune response and its durability against cancer.
What is PT-112’s osteotropism. How does this property influence its effectiveness in treating cancers affecting the bone, such as metastatic castration-resistant prostate cancer?
Dr. Johan Baeck: At recent medical conferences, we’ve shared cases of patients from our phase 1 and phase 2 studies exhibiting long-lasting responses, suggesting our treatments may enhance immune memory. This observation aligns with the decade-long understanding that some patients achieve prolonged survival benefits, potentially indicating curative outcomes.
These findings have prompted further investigation, as we are currently analyzing extensive data from our phase 2 study to draw more definitive conclusions. Notably, PT-112 has demonstrated efficacy in metastatic castrate-resistant prostate cancer, achieving active concentrations in both soft tissues and bones. This dual-targeting capability addresses significant challenges in patient treatment, highlighting our drug’s potential across different cancer environments.
In prostate cancer, a significant number of patients develop symptomatic bone metastases, leading to pain or fractures due to tumor growth in the mineralized bone. PT-112, with its pyrophosphate structure, uniquely targets these areas, demonstrating a higher affinity for bone tissues in preclinical studies. This specificity allows PT-112 to concentrate in the bone, affecting the mineralized shell while sparing the bone marrow.
This approach minimizes adverse effects such as fractures and does not harm the bone marrow, where critical blood cells are produced, thereby reducing the risk of anemia, thrombocytopenia, or neutropenia. Furthermore, our clinical studies in phases 1 and 2 have shown promising results.
Patients with high levels of the biomarker alkaline phosphatase, which correlates with bone metastases, experienced significant reductions in levels after treatment with PT-112. This reduction is associated with improved overall survival, a trend we observed in our research, suggesting PT-112’s potential for positively impacting survival in prostate cancer patients with bone metastases.
Safety and tolerability are critical aspects of any cancer therapy. What has been observed regarding the safety profile of PT-112 in clinical trials?
Dr. Johan Baeck: In our comprehensive phase 1 and phase 2 studies, we’ve established that PT-112 is well-tolerated across the board. This is particularly significant for our late-line patient population, who have undergone extensive prior treatments, including chemotherapy, and are often in a frail condition. Despite their vulnerability, our treatment does not significantly increase adverse events, with most observed side effects being mild (grade 1 and 2).
PT-112 is currently in Phase 2 trials for metastatic castration-resistant prostate cancer and in collaboration with the NCI for thymoma and thymic carcinoma. Can you provide an update on these trials and any preliminary results?
Dr. Johan Baeck: Focusing on our collaboration with the NCI on rare cancers like thymic cancer, the ongoing phase 2 study is showing promising preliminary safety results, showing no new immune-related adverse events. This is particularly relevant given the potential autoimmune challenges these patients may face.
Preliminary efficacy data are encouraging with 9 out of 11 patients to date presenting with stable disease or better. Our findings underscore our commitment to safety, especially in treatments targeting immune responses in already vulnerable populations.
In metastatic castrate-resistant prostate cancer, PT-112 has been well-tolerated, with early trends suggesting a survival benefit compared to existing available treatments. Given these patients often lack effective standard of care options, our results are notably encouraging. We anticipate further efficacy data by the end of 2024, which will inform our regulatory strategy for late-stage development and phase 3 trials.
The combination therapy of PT-112 with avelumab, a PD-L1 checkpoint inhibitor, showed promise in early trials. How do you evaluate the results of these combination therapies?
Dr. Johan Baeck: Our priority is ensuring that PT-112 is safe and well-tolerated in combination therapies, a goal we’ve successfully met. We’ve also proven that its mechanism of action complements that of its combination partners. This compatibility has been particularly promising in our studies, suggesting potential for broader applications, like early-line prostate cancer treatment.
PT-112 having received orphan drug designations, what are the next steps in its clinical development, and what timelines are you aiming for in terms of regulatory approvals?
Dr. Johan Baeck: We’ve secured orphan drug designation for our treatment in thymic cancers and multiple myeloma, highlighting significant opportunities in areas in need of improved treatment options. We’re encouraged by our collaboration with the NCI on studies for thymic cancers, currently exploring monotherapy.
Although these studies are ongoing, initial findings presented at ASCO show promising trends. We’re keenly awaiting further data to refine our understanding of the treatment’s safety and efficacy, guiding our strategic approach to these rare cancers.
How does Promontory plan to expand its pipeline beyond PT-112, particularly in targeting other challenging cancers?
Dr. Johan Baeck: In our phase 1 and 2 studies, we’ve demonstrated that small molecules with immune response properties have a significant role in oncology, guiding our company’s direction. Our approach, unlike targeting specific subpopulations requiring particular mutations, applies broadly across various indications and patient groups. This positions us as pioneers in developing small molecules that enhance immune responses, with our lead drug at the forefront of this exciting new field.
Are there other partnerships or collaborations on the horizon that could accelerate the development of your cancer therapies?
Dr. Johan Baeck: We are actively engaging with biopharma companies in US and EU to advance our PT-112 program, a testament to our commitment. Collaborating closely with organizations like the NCI underscores our strategic approach.
Additionally, our expansion into France by opening trial sites last year aims to enhance patient enrollment. Through our involvement with the Paris-Saclay Cancer Cluster, initiated by President Macron’s vision to position France as a competitive hub in cancer research, we’ve become the first international company to join this endeavor.
This affiliation is not just a milestone for us but also a strategic move to bolster our Phase 3 trial preparations, ensuring a robust presence ac-ross Europe. Such strategic partnerships and expansions are crucial, especially considering the importance of European sites in global Phase 3 trials, marking an exciting and significant step in our development efforts.


Comments
No Comments Yet!