Oncolytic Virus-Based Gene Therapy Enhances Survival in Brain Cancer

ONCOLife |
20 October 2023
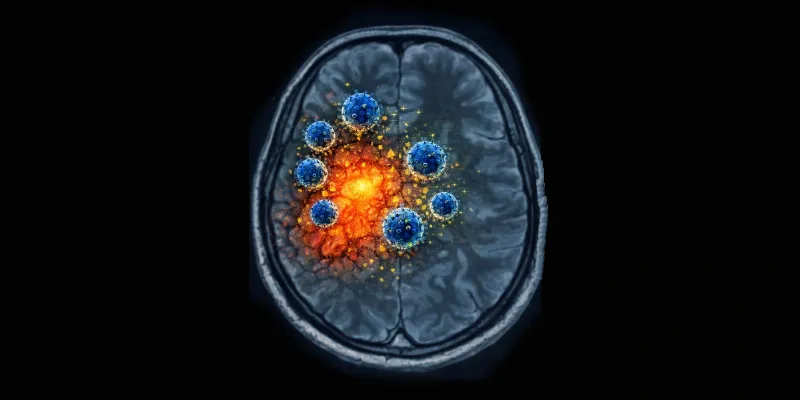
Researchers at Mass General Brigham have developed a promising gene therapy to treat aggressive brain cancer, as reported in a new study published in Nature. They utilized a modified oncolytic herpes simplex virus to transform the tumor's protective environment, allowing the immune system to attack. The results suggest that gene therapy is predominantly safe and extended survival rates.
The trials indicate that the oncolytic virus CAN-3110 could boost survival rates for patients with recurrent glioblastoma (GBM), an aggressive brain cancer resistant to existing treatments. In a phase 1 trial with 41 patients, the treatment notably prolonged survival for those with pre-existing viral antibodies. This innovative gene therapy approach offers hope for brain cancer patients.
“GBM has an aggressive effect in part because of a milieu of immunosuppressive factors surrounding the tumor, which enable the tumor’s growth by preventing the immune system from entering and attacking it. This study showed that with a virus we designed, we can reshape this ‘immune desert’ into a pro-inflammatory environment,” said corresponding author of the study, E. Antonio Chiocca.
Differing from other oncolytic herpes simplex viruses used clinically, CAN-3110 contains the ICP34.5 gene, often omitted due to its potential to cause human diseases. Researchers believed that this gene might be crucial in stimulating a robust, pro-inflammatory reaction necessary to combat the tumor. As a result, they created a variant of the virus that included the ICP34.5 gene but was also specifically designed to spare healthy brain cells.
The trial, which tested CAN-3110's safety on 41 patients with high-grade gliomas, including 32 with recurrent GBM, found it to be largely safe. Only two participants experienced seizures as a severe adverse event. Impressively, GBM patients with pre-existing antibodies against the HSV1 virus (comprising 66% of the participants) witnessed a median overall survival of 14.2 months.
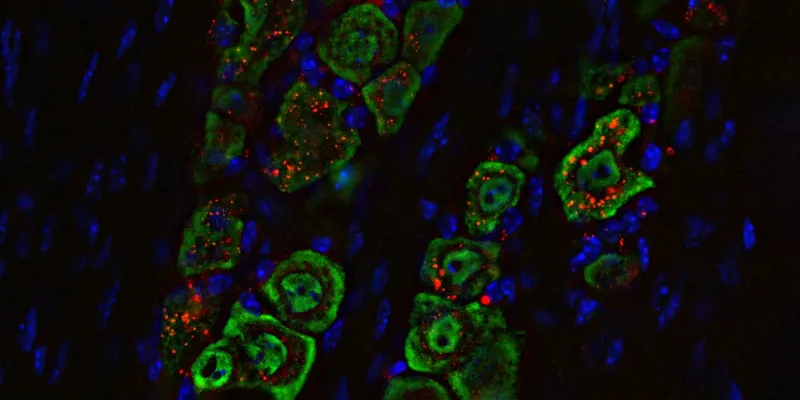
These patients also displayed notable changes in the tumor microenvironment, indicating immune activation. Following the treatment, a marked increase in the diversity of T cells was observed, implying a broad immune response that might be a result of the virus eliminating tumor cells and releasing cancer antigens. These immunological shifts post-treatment correlated with better survival outcomes.
This innovative gene therapy approach offers a beacon of hope for GBM patients. The Mass General Brigham's Gene and Cell Therapy Institute aims to push this frontier further by turning groundbreaking scientific discoveries into first-in-human clinical trials, leading to transformative treatments for patients.
“Almost no immunotherapies for GBM have been able to increase immune infiltration to these tumors, but the virus studied here provoked a very reactive immune response with infiltration of tumor-killing T-cells. That’s hard to do with GBM, so our findings are exciting and give us hope for our next steps,” Chiocca said.
The researchers are now setting their sights on further studies to assess the oncolytic virus's effectiveness in patients with and without HSV1 antibodies. With the safety of a single viral injection established, they are gearing up to evaluate the safety and efficacy of up to six injections over four months. This iterative approach, akin to multiple vaccination rounds, might amplify the therapy's potency.
Abstract of the research
Clinical trial links oncolytic immunoactivation to survival in glioblastoma
Abstract: Immunotherapy failures can result from the highly suppressive tumour microenvironment that characterizes aggressive forms of cancer such as recurrent glioblastoma (rGBM)1,2. Here we report the results of a first-in-human phase I trial in 41 patients with rGBM who were injected with CAN-3110—an oncolytic herpes virus (oHSV)3. In contrast to other clinical oHSVs, CAN-3110 retains the viral neurovirulence ICP34.5 gene transcribed by a nestin promoter; nestin is overexpressed in GBM and other invasive tumours, but not in the adult brain or healthy differentiated tissue4. These modifications confer CAN-3110 with preferential tumour replication. No dose-limiting toxicities were encountered. Positive HSV1 serology was significantly associated with both improved survival and clearance of CAN-3110 from injected tumours. Survival after treatment, particularly in individuals seropositive for HSV1, was significantly associated with (1) changes in tumour/PBMC T cell counts and clonal diversity, (2) peripheral expansion/contraction of specific T cell clonotypes; and (3) tumour transcriptomic signatures of immune activation. These results provide human validation that intralesional oHSV treatment enhances anticancer immune responses even in immunosuppressive tumour microenvironments, particularly in individuals with cognate serology to the injected virus. This provides a biological rationale for use of this oncolytic modality in cancers that are otherwise unresponsive to immunotherapy (ClinicalTrials.gov: NCT03152318).


Comments
No Comments Yet!