UC Davis Scientists Discover 'Death Switch' to Triggering Cancer Cell Self-Destruction

ONCOLife |
29 October 2023
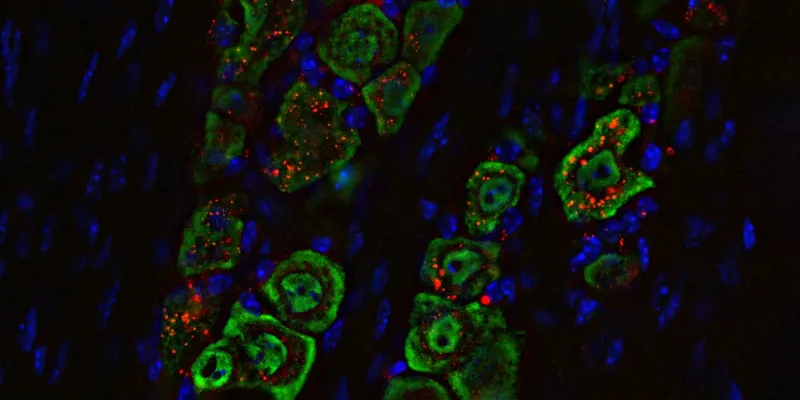
Scientists have discovered an epitope on the CD95 receptor that can trigger cancer cells to self-destruct. This discovery could enhance the efficacy of current immunotherapies, revolutionize solid tumor treatments, and offer promising new cancer therapies.
Recent research breakthroughs have pointed to a promising direction in cancer therapy. Scientists from the UC Davis Comprehensive Cancer Center have identified a specific section on the CD95 receptor, also known as Fas, which could potentially instruct cancer cells to self-destruct. This finding, published in the Nature journal Cell Death & Differentiation, heralds a potential revolution in the treatment of solid tumors.
The CD95 receptor, aptly termed the 'death receptor', plays a pivotal role in the process. When this receptor is activated, it initiates a signal, instructing cells to self-destruct, a phenomenon experts believe can be harnessed to develop more effective cancer treatments.
Jogender Tushir-Singh, the senior author of the study and an associate professor in the Department of Medical Microbiology and Immunology at UC Davis, shared,
“We have found the most critical epitope for cytotoxic Fas signaling, as well as CAR T-cell bystander anti-tumor function. Previous efforts to target this receptor have been unsuccessful. But now that we’ve identified this epitope, there could be a therapeutic path forward to target Fas in tumors.”
Traditional cancer treatments, such as surgery, chemotherapy, and radiotherapy, can be effective initially. However, there is a challenge with therapy-resistant cancers that often re-emerge. Immunotherapies, particularly CAR T-cell-based therapies, have shown significant promise in disrupting this recurrence cycle.
These therapies involve engineering a patient's T-cells to target and attack tumor cells. While they've demonstrated success against blood cancers like leukemia, their efficacy against solid tumors has been limited. These solid tumors, often referred to as "cold tumors", are adept at shielding themselves from immune cells.
Tushir-Singh explained the challenge, “These are often called cold tumors because immune cells simply cannot penetrate the microenvironments to provide a therapeutic effect. It doesn’t matter how well we engineer the immune receptor activating antibodies and T cells if they cannot get close to the tumor cells. Hence, we need to create spaces so T cells can infiltrate.”
The discovery of the CD95 epitope could be the answer. By targeting this epitope, scientists believe they can not only destroy tumor cells but also enhance the efficacy of existing immunotherapies, particularly CAR T-cell therapy. This dual-action mechanism could provide a powerful weapon against tumors.
Furthermore, the study highlighted the importance of understanding a patient's Fas status. Tushir-Singh emphasized,
"This is a definitive marker for bystander treatment efficacy of CAR T therapy. But most importantly, this sets the stage to develop antibodies that activate Fas, selectively kill tumor cells, and potentially support CAR T-cell therapy in solid tumors."
This knowledge could serve as a marker for the treatment's effectiveness and help design strategies to boost CAR T-cell therapy's impact on solid tumors. While the research is still in its early stages, the findings offer a beacon of hope. The next steps involve developing antibodies that can target this epitope, potentially unlocking a new era in cancer treatment.
Abstract of the research
Characterizing the regulatory Fas (CD95) epitope critical for agonist antibody targeting and CAR-T bystander function in ovarian cancer
Abstract: Receptor clustering is the most critical step to activate extrinsic apoptosis by death receptors belonging to the TNF superfamily. Although clinically unsuccessful, using agonist antibodies, the death receptors-5 remains extensively studied from a cancer therapeutics perspective. However, despite its regulatory role and elevated function in ovarian and other solid tumors, another tumor-enriched death receptor called Fas (CD95) remained undervalued in cancer immunotherapy until recently, when its role in off-target tumor killing by CAR-T therapies was imperative. By comprehensively analyzing structure studies in the context of the binding epitope of FasL and various preclinical Fas agonist antibodies, we characterize a highly significant patch of positively charged residue epitope (PPCR) in its cysteine-rich domain 2 of Fas. PPCR engagement is indispensable for superior Fas agonist signaling and CAR-T bystander function in ovarian tumor models. A single-point mutation in FasL or Fas that interferes with the PPCR engagement inhibited apoptotic signaling in tumor cells and T cells. Furthermore, considering that clinical and immunological features of the autoimmune lymphoproliferative syndrome (ALPS) are directly attributed to homozygous mutations in FasL, we reveal differential mechanistic details of FasL/Fas clustering at the PPCR interface compared to described ALPS mutations. As Fas-mediated bystander killing remains vital to the success of CAR-T therapies in tumors, our findings highlight the therapeutic analytical design for potentially effective Fas-targeting strategies using death agonism to improve cancer immunotherapy in ovarian and other solid tumors.


Comments
No Comments Yet!