A Breakthrough in Personalizing Lung Cancer Therapy with the GO Chip for Tumor Monitoring


ONCOLife |
4 March 2025
The innovative GO chip, developed at the University of Michigan, represents a significant leap in lung cancer treatment by enabling precise monitoring of treatment responses. In this exclusive ONCOLife interview, Dr. Shruti Jolly and Prof. Sunitha Nagrath discuss their groundbreaking research, focusing on the chip’s ability to detect changes in circulating tumor cells (CTCs) and its potential to transform cancer therapy through personalized adjustments.
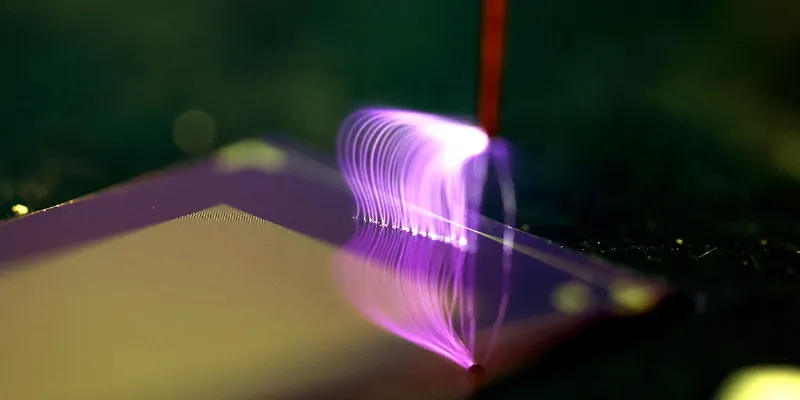
The GO chip, integrating graphene oxide nanosheets within a microfluidic platform, promises to advance how we monitor and personalize cancer treatment. This technology not only captures a broad spectrum of tumor cell subtypes but also allows for early intervention by pinpointing ineffective treatments, potentially reducing unnecessary exposure to them.
Click the picture to view the PDF version: Pg 24-27.
How the GO Chip Could Advance Lung Cancer Treatment
How could the GO chip transform lung cancer treatment monitoring and reduce the assessment period for treatment efficacy?
Dr. Jolly: Our study on stage-III lung cancer patients aimed to personalize treatments based on individual responses. Initially, the standard was chemotherapy and radiation, later augmented by immunotherapy with durvalumab. We sought to use radiographic and blood biomarkers to optimize radiation levels for each patient.
Collaborating with Prof. Nagrath’s lab, we incorporated the GO chip, a microfluidic platform integrating graphene oxide nanosheets. This platform isolates cancer cells with remarkable precision, addressing the limitations of traditional technologies like CellSearch, which struggled with the heterogeneity of lung cancer CTCs. The GO chip’s antibody cocktail enables the capture of diverse tumor cell subtypes, providing a nuanced approach to monitoring tumor dynamics and treatment responses.
How does the GO chip’s specificity and sensitivity compare to existing FDA approved methods for detecting CTCs in lung cancer?
Prof. Nagrath: Graphene oxide technology excels in capturing CTCs even at early stages, enabling tailored treatments. Unlike traditional methods, the GO chip provides insights into treatment efficacy early in the course of therapy, allowing timely adjustments. This clinical trial, designed for adaptive radiation treatment, validated the GO chip’s capabilities in a real-world setting.
The process is streamlined: blood samples are collected in EGTA tubes, processed immediately in the lab, and analyzed for dynamic CTC changes. This approach enhances accuracy, ensuring that the data correlates closely with treatment responses or resistance, enabling more proactive management strategies.
Can you explain the technology behind the GO chip and challenges faced during its development?
Prof. Nagrath: Existing microfluidic technologies primarily targeted metastatic cancers with higher CTC counts. For stage-III cancers, where CTCs are fewer, we needed a solution capable of isolating even minimal numbers of cells. The GO chip’s graphene oxide nanosheets provide a high surface area for effective cell capture.
Challenges included functionalizing the graphene oxide with antibodies and optimizing flow rates to achieve high purity. Purity is crucial for downstream molecular analyses, such as RNA extraction and transcriptomic profiling. This precision is essential for understanding treatment resistance and refining therapeutic strategies.
Why is using multiple protein markers superior to single-marker approaches in lung cancer?
Prof. Nagrath: Single-marker methods often fail in lung cancer due to the low expression of typical markers like EpCAM. The GO chip overcomes this by employing a cocktail of antibodies, including EGFR and CD133, which capture a broader range of CTC subtypes. This multiplex approach significantly enhances the chip’s efficiency and makes it uniquely suited for lung cancer, unlike technologies designed for other cancer types.
How might findings from non-responsive treatments influence the development of targeted therapies for lung cancer?
Prof. Nagrath: Integrating GO chip data with next-generation sequencing (NGS) offers a dynamic view of the tumor’s genomic landscape. Unlike NGS, which is limited to single biopsies, the GO chip provides continuous monitoring of tumor evolution.
This synergy allows for more precise and adaptive therapies, addressing treatment resistance more effectively. From a technology perspective, a sensitive and rapid blood test could revolutionize clinical practice, offering real-time insights into genomic changes and directly influencing treatment decisions.
How could GO chip’s integration into routine practice affect patient management?
Dr. Jolly: Before clinical adoption, we need further validation with larger patient cohorts. Early signals from our study indicate strong potential for optimizing radiation timing and dosage. For instance, initiating analysis at two weeks instead of four weeks could provide even earlier insights into treatment efficacy, allowing real-time personalization of therapy.
Unlike PET scans, which have slower response times, the GO chip offers immediate feedback, revolutionizing adaptive treatment strategies and reducing unnecessary side effects.
What are the current stages of clinical trials, and how do you plan to validate the GO chip further?
Prof. Nagrath: Our proof-of-concept study involved 26 patients monitored across six time points over three years. Moving forward, we aim to expand trials to include larger, more diverse cohorts. Additionally, gathering real-world data will help refine the technology’s applicability and establish its role in routine cancer management.
Potential Impact on Clinical Outcomes
Dr. Jolly: Early identification of ineffective treatments can significantly improve patient outcomes by reducing unnecessary exposure to side effects and financial burdens. Although it’s premature to quantify the full impact, the GO chip’s ability to provide actionable insights early in the treatment process could lead to substantial advancements in personalized oncology care.
This groundbreaking collaboration between Prof. Jolly and Prof. Nagrath exemplifies how interdisciplinary research can drive transformative progress in oncology. The GO chip is a testament to the power of innovation in improving patient care and advancing precision medicine.











Comments
No Comments Yet!