How Novel Immunotherapy IMNN-001 Could Change Ovarian Cancer Outcomes


ONCOLife |
25 November 2024
The groundbreaking results of the OVATION 2 Study demonstrated a substantial 35% improvement in overall survival, equating to nearly a year of extended life beyond current standards. In this exclusive ONCOLife interview, Dr. Stacy Lindborg, CEO of IMUNON, and Dr. Premal Thaker, Professor in Obstetrics and Gynecology and Interim Chief of Gynecologic Oncology at Washington University, provide an in-depth overview of the OVATION 2 Study, highlighting clinical advancements in ovarian cancer treatment.
The Findings of the OVATION 2 Study
Dr. Lindborg and Dr. Thaker discuss the integration of IMNN-001, a pioneering immunotherapy, with standard chemotherapy and PARP inhibitors, highlighting its promising efficacy. IMNN-001, a novel immunotherapy, demonstrates significant improvements in progression-free and overall survival rates.
Click the picture to view the PDF version: Pg 32-36.
Could you begin by sharing the latest positive topline data from the OVATION 2 study? What were the key findings?
Dr. Lindborg: In our Phase 2 trial for newly diagnosed ovarian cancer patients, we used a neoadjuvant treatment followed by debulking surgery and adjuvant therapy. Our intent-to-treat population demonstrated a hazard ratio of 0.74, indicating a 35% improvement in overall survival when using IMNN-001 plus standard-of-care, which is platinum-based chemotherapy, combination of paclitaxel and carboplatin (NACT), compared to using NACT alone.
The median overall survival in the experimental group, where IMNN-001 was combined with NACT, extended by almost a year. Specifically, while the standard-of-care treatment arm showed a median survival of 29 months, the experimental treatment arm exhibited a survival of 40 months. Given that a survival benefit has not ever been observed in ovarian cancer, these results are highly significant.
We observed even more compelling data among subgroups, especially in women who received a higher number of treatment cycles of IMNN-001. For instance, those who received at least three doses of the experimental treatment and at least one cycle of chemotherapy saw the hazard ratio decrease to 0.64, with an extension of median overall survival by 15.7 months -a 56% improvement over standard care.
Additionally, the use of PARP inhibitors as part of maintenance therapy further enhanced outcomes. In patients treated with IMNN-001 and chemotherapy, the hazard ratio dropped significantly to 0.41 in those who received PARP inhibitors. The median overall survival for this subgroup has not yet been reached, contrasting with a median survival of 37 months in those treated with PARP inhibitors under the standard of care.
These results, including progression-free survival, are very encouraging. They not only reflect a meaningful improvement but also show consistency across various endpoints and subgroups. This consistency brings great hope and excitement that these results can be replicated in Phase 3, marking a significant advancement in the treatment landscape for ovarian cancer.
Dr. Thaker: The results from Ovation 2, integrating immunotherapy with standard chemotherapy for ovarian cancer, show that we’ve achieved significant progress. This is the first immunotherapy treatment demonstrating benefits in both progression-free and overall survival. Particularly exciting is the synergy with PARP inhibitors, which have transformed treatment but still leave many women uncured.
Our data suggest improved survival rates due to this synergy, marking a potential shift in standard of care. This advancement could benefit not only patients with HRD and BRCA mutations but also the broader intent-to-treat population, which currently has limited options. This breakthrough offers hope for extending benefits to more women in the future.
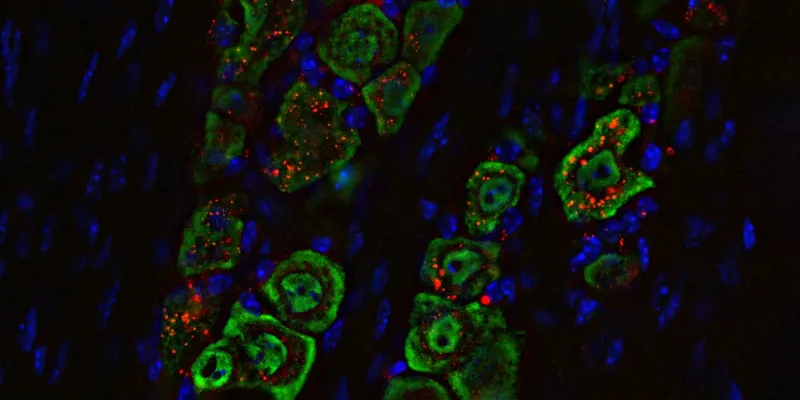
IMNN-001 leverages IL-12 via TheraPlas technology. Can you explain the mechanism by which IL-12 enhances anticancer immunity in the context of ovarian cancer?
Dr. Thaker: IL-12 is a powerful cytokine crucial in mounting an immune response, but its use has been limited due to severe side effects from previous delivery methods using humanized monoclonal antibodies. With our new DNA plasmid technology, we can produce IL-12 locally within the tumor microenvironment, significantly reducing side effects like fever and cytokine release syndrome.
This advancement allows us to harness IL-12’s benefits—boosting both adaptive immunity and anti-angiogenic mechanisms—important for fighting cancer, without the adverse effects. After decades of research, we’ve finally developed a method to safely administer IL-12 to patients.
Dr. Lindborg: Reflecting on past learning and attempts, we’ve significantly progressed in safely delivering IL-12 directly into the tumor environment. IMNN-001 utilizes a DNA plasmid delivery system that protects DNA from degradation and enhances cellular uptake without excessive breakdown. This method increases the durability of IL-12, extending its impact, which aligns with the survival outcomes we’re observing.
IL-12 functions through paracrine and autocrine mechanisms, targeting immune cells within the tumor and adjacent lymph nodes, not circulating lymphocytes. By focusing on the local tumor milieu and optimizing IL-12 delivery, we are maximizing safety and potentially driving robust anti-tumor responses.
How long do women with advanced ovarian cancer typically live on current standard of care therapy? How have PARP inhibitors changed that?
Dr. Thaker: We are striving to make ovarian cancer a chronic, manageable disease, using various agents to improve outcomes. Ultimately, our goal is to cure patients and prevent recurrence. We aim to integrate effective molecules like chemotherapies and other agents early in treatment. Previously, combinations like bevacizumab with taxol and carboplatin didn’t improve overall survival.
However, we’re now seeing significant overall survival benefits with the immunotherapy IMNN-001, which shows promise across all patients. Particularly, there’s notable synergy when used with PARP inhibitors, which have significantly helped a specific patient group. This progress is crucial as we work to enhance the immune environment and benefit a broader population of ovarian cancer patients.
Could you discuss the IMNN-001 safety profile observed during the OVATION 2 study? IL-12 has a history of adverse events and intolerability, how does IMNN-001 overcome these issues?
Dr. Thaker: In the OVATION 2 trial, we observed side effects like myelosuppression, including decreased white co-unts and hemoglobin levels. However, frequent lab checks helped us manage these effectively, as regular monitoring is common in chemotherapy and doesn’t pose an insurmountable issue.
We also saw abdominal pain from intra-abdominal delivery, but we effectively managed this with pain and anti-anxiety medications. Importantly, patients benefitted from IMNN-001, particularly when they received at least 20% of the prescribed dose, demonstrating early positive changes with our treatment administration.
What are the unmet needs for women with advanced ovarian cancer? What is the market potential of IMNN-001 considering other treatments are available or in development?
Dr. Thaker: There’s a significant unmet need in treating ovarian cancer, the second deadliest gynecologic malignancy. Most new treatments target later stages rather than the initial diagnosis where the therapeutic impact could be greatest. The promising results from the OVATION 2 study have us hopeful, and we’re excited to see if the upcoming Phase 3 trial, OVATION 3, will continue to show such encouraging outcomes.
Dr. Lindborg: According to the International Agency of Research on Cancer, there are about 300,000 global diagnoses of ovarian cancer annually, with around 20,000 in the US alone, as reported by the American Cancer Society.
Assuming 80% are newly diagnosed and eligible for neo-adjuvant regimen treatment, there’s a significant market for our experimental treatment, IMNN-001. This treatment shows promising benefits across a broad intent-to-treat population, which is not only intriguing from a market perspective but also holds substantial potential from a human standpoint.
As you prepare for the Phase 3 study, what specific endpoints or modifications are you considering based on the learnings from OVATION 2?
Dr. Lindborg: The trial design for our upcoming study will closely resemble the OVATION 2 trial, as is typical in confirmatory trials. However, significant modifications will stem from our learnings from the current phase. This was our first time studying IMNN-001 in both neoadjuvant and adjuvant settings, which provided a rich environment for insights.
Notably, we’ll adjust the primary endpoint to focus on overall survival based on the impressive responses observed. We also plan to stratify participants by HRD and HRP to ensure balanced treatment arms, especially considering genetic mutations and responses to PARP inhibitors.
Additionally, we’ve implemented a prophylactic pain protocol in the Phase 2 trial, significantly improving patient comfort and treatment adherence. This protocol will be essential in the next phase, ensuring we offer the best possible treatment and setting the trial up for success.


Comments
No Comments Yet!