Location of T Cells Could Revolutionize Immunotherapy Success in Lung Cancer
1 September 2023
The University of Edinburgh's research suggests that the positioning of certain immune cells within lung tumours could predict patient survival and treatment response. This could enhance the efficacy of immunotherapies, which currently fail in 80% of lung cancer cases. The study focused on cytotoxic T cells and found that enzymes CD39 and CD73, associated with reduced patient survival, are exploited by tumours to evade destruction.
Notably, high levels of CD39 in tumour nests indicated better patient outcomes. Insights from this research could potentially guide treatments, determining which patients might benefit from immunotherapies and identifying those who might not. The survival rates and responses to treatment in lung cancer patients might be better predicted by examining the location of certain immune cells within tumours, according to a breakthrough study by the University of Edinburgh.
Lung cancer, a leading cause of cancer-related deaths globally, is often diagnosed at an advanced stage where conventional treatments are typically less effective. While immunotherapies have revolutionised treatment, they are currently ineffective in 80% of cases. The study has been published in the Journal for Immunotherapy of Cancer. This research offers a deeper comprehension of why some patients benefit more than others.
Dr. Ahsan Akram, from the University of Edinburgh’s Centre for Inflammation Research, remarked, “This study helps us to understand that we need to know the types of T cells in the cancer and their location within the tumors to begin to appreciate the complexity we are dealing with. We hope these results will lead to more research in this area, and in the future could help to identify patients who will do well with immunotherapies, as well as identifying earlier those that may not, so alternative treatments can be tried.”
This research could improve the success of immunotherapies
The Cancer Research UK-funded study focussed on cytotoxic T cells – white blood cells pivotal in tackling cancer. The team analysed tumour tissue from 162 patients with non-small cell lung cancer (NSCLC), responsible for over 80% of lung cancer cases. They discovered that two enzymes, CD39 and CD73, if found near tumours, were linked with reduced patient survival. These enzymes play a role in preventing T cells from becoming overly active; however, tumours can exploit this mechanism to avoid destruction.
Significantly, it was observed that high levels of CD39 within clusters of cancer cells, or tumour nests, correlated with better patient survival and a more positive reaction to immunotherapy. Conversely, when these cells were located outside these clusters, patient survival was not impacted. Furthermore, elevated levels of CD39 on regulatory T cells, which generally stop the immune system from overreacting, were tied to decreased survival.
Abstract of research
Location of CD39+ T cell subpopulations within tumors predict differential outcomes in non-small cell lung cancer
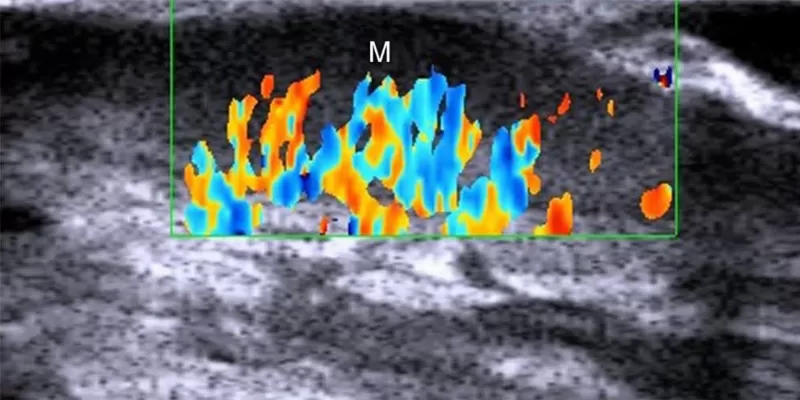
Abstract - Purpose: An improved mechanistic understanding of immunosuppressive pathways in non-small cell lung cancer (NSCLC) is important to develop novel diagnostic and therapeutic approaches. Here, we investigate the prognostic significance of the ectonucleotidases CD39 and CD73 in NSCLC. Results: We demonstrate that flow cytometry of early untreated NSCLC patients shows an upregulation of CD39 expression in the tumor tissue among natural killer (NK) cells, fibroblasts and T cells. CD73 expression is mainly found among fibroblasts and Epcam+cells in the tumor tissue. Multiplex Immunofluorescence in a cohort of 162 early untreated NSCLC patients demonstrates that CD39 expression is mainly localized in the tumor stroma while CD73 expression is equally distributed between tumor nest and stroma, and high expression of CD39 and CD73 in the tumor stroma is associated with poor recurrence-free survival (RFS) at 5 years. Additionally, we find that CD8+T cells located in the tumor nest express CD103 and the density of CD39+CD103+CD8+ T cells in the tumor nest predicts improved RFS at 5 years. Targeted RNA-Seq shows that the tumor microenvironment of NSCLC upregulates regulatory pathways in CD4+ T cells and exhaustion in CD8+ T cells, and analysis of a single cell RNA sequencing dataset shows that CD39+CD4+ cells are enriched in Treg signature gene-sets, and CD39+CD103+ cytotoxic T lymphocyte show gene signatures indicative of an exhausted cytotoxic phenotype with upregulated expression of CXCL13. Conclusions: Knowledge of patterns of distribution and location are required to understand the prognostic impact of CD39+ T cell populations in NSCLC. This study provides an improved understanding of spatial and functional characteristics of CD39+ T cells and their significance to patient outcome.





Comments
No Comments Yet!