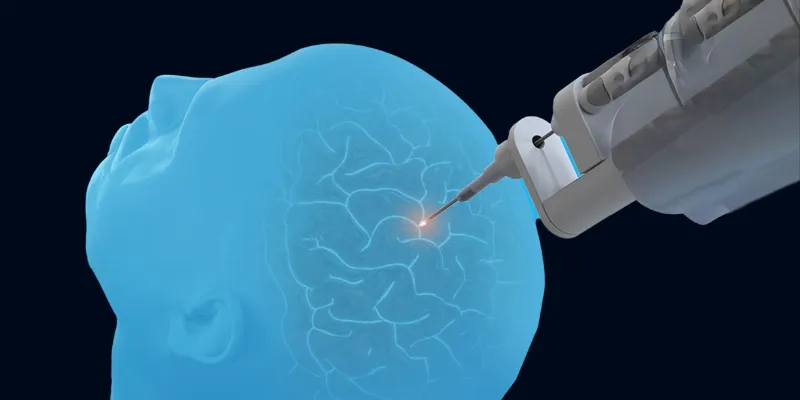
Elevating Safety and Efficacy in Brain Tumor Treatment with the NB3 Laser Probe

ONCOLife |
23 July 2024
Pioneering new laser probe could play a revolutionary role in the treatment of brain cancers. Marty Emerson, CEO of Monteris Medical, answers our questions on this innovative technology for ONCOLife, and discusses the advancements of the NeuroBlate NB3 FullFire 1.6mm Probe, the smallest brain surgery laser probe to date. Emerson highlights the probe’s precision and minimal invasiveness, which are pivotal in improving outcomes for pediatric and oncological neurosurgery.
Click the picture to view the PDF version: Pg 13-17.
Exclusive Interview with Marty Emerson
The NeuroBlate NB3 FullFire 1.6mm Probe is a pioneering device that promises a new trend in treating brain cancer, including pediatric tumors. Marty Emerson emphasizes the integration of advanced cooling technology and the probe’s significant role in enhancing the safety and efficacy of brain tumor treatments, marking a transformative step forward in neurosurgical practices.
How does the NeuroBlate FullFire Laser Probe differentiate itself from other commercially available laser probes? Can you provide a general overview of its features?
Emerson: Physicians have expressed a need for the smallest possible probe that still delivers the largest ablation feasible in the brain, ideally around 3 centimeters, due to constraints like the skull’s hardness and potential post-procedure swelling. Our NB3 probe, at just 1.6 millimeters and featuring cooling technology, hits the perfect balance.
It’s the smallest probe capable of delivering significant energy, and in early uses, it’s achieving near the 3-centimeter ablation limit. This optimization allows for the largest ablations and, through our software’s precision, very small ablations as needed, particularly in pediatric cases where sizes might range from 4 to 6 millimeters. We are now confidently achieving this wide range of ablations.
Can you elaborate on the cooling technology incorporated into the NB3 probe and how it contributes to its efficacy in treating brain tumors
Emerson: Since our inception, all NeuroBlate laser pro-bes have been specifically designed for brain use, unlike many competitors’ probes, which were initially intended for other organs like the prostate.
Our focus was to create probes suitable for the brain, featuring cooling technology that operates seamlessly behind the scenes. Probe cooling is completely transparent to the surgeon, who activates the laser with a pedal.
The sophistication lies in our software, which simultaneously monitors temperature, adjusts cooling levels, and modulates laser power to optimize tissue ablation. This is not just a technical achievement but a practical solution to a significant challenge in laser ablation—managing the heat generated during the procedure.
The rationale behind this is crucial: excessive heat at the probe’s surface can cause tissue charring, which hinders effective heat distribution necessary for achieving a large and safe ablation target, up to 3 centimeters. Thus, active cooling is essential for allowing heat to be effectively and safely propagated, ensuring precise and predictable ablation outcomes.
Can you discuss the prospective clinical evidence supporting the efficacy of the NeuroBlate System, particularly in brain tumor treatment outcomes? How has it been shown to affect patient quality of life?
Emerson: We’ve led the collection of compelling prospective data on the use of NeuroBlate laser ablation on more than 1,000 patients through our LAANTERN multi-center study. Our focus is on demonstrating that laser interstitial thermal therapy (LITT) can achieve comparable cancer control outcomes while significantly enhancing the patient’s quality of life and reducing recovery time.
Published evidence from LAANTERN shows that laser ablation can achieve a comparable extent of resection to craniotomy, with much quicker recovery times. Post-procedure recovery for patients undergoing traditional resective surgery versus those opting for our less invasive LITT are dramatic.
Traditional surgery involves removing a substantial part of the patient’s skull and then replacing it, leading to a lengthy and significant recovery process, including extended stays in the ICU. In contrast, with LITT, the procedure involves making a small opening about the diameter of a pencil in the brain.
Patients can often go home the next day, requiring only one or two stitches and have little or no pain, showcasing a dramatic difference in recovery time. For the oncology patient population with pos-sibly limited time, a short recovery is critical. We are also proud to have the first randomized controlled trial on laser ablation for progressive metastatic disease, called REMASTer.
Led by Duke University, we are now enrolling in this important study that investigates LITT using NeuroBlate as an early intervention for radiographically progressive brain metastases and to provide Level I evidence to guide treatment for this complex patient population.
What patient segments and clinical benefits does the NB3 probe offer that are not available with other laser probes?
Emerson: Our primary focus with the NB3 has been on pediatric neurosurgery, given the critical importance of minimizing invasiveness for these patients. This probe was specifically designed with children in mind, where smaller is definitively better.
This is especially true when navigating the probe through eloquent, highly sensitive brain areas, where reducing the probe’s diameter minimizes potential side effects. However, the early performance of this probe has exceeded our initial expectations, suggesting a broader application than we initially anticipated.
This is encouraging because neurosurgeons universally prefer the smallest, least invasive tools that can achieve the largest possible ablation. Our experiences indicate that our 1.6 millimeter probe will likely be widely adopted beyond pediatric applications, similar to ot-her neurosurgical technologies like deep brain stimulation and stereotactic surgery leads, which are about the same size and have been readily incorporated into practice.
We are very optimistic about the applicability of our technology across various patient groups, despite originally envisioning a more narrow usage. Could you explain the significance of the NB3 probe’s adaptability in multi-trajectory procedures for brain tumor surgery?
Emerson: Our probe technology significantly enhances both economic value and workflow efficiency. With our design, a physician can insert multiple trajectories in the brain during a single surgical session and use the same probe to ablate in each of these entry points, so hospitals save on probe costs.
Plus, unlike our previous models with several probe lengths to accommodate var-ying lesion depths, NB3 is a single length, capable of reaching both shallow and deep targets. This versatility simplifies the procedure and reduces hospital inventory.
How do Monteris’ leading software and robotics enhance the precision and flexibility of the NB3 probe during neurosurgical procedures?
Emerson: The NB3 probe’s precision is crucial for treating conditions like epilepsy or tumors near eloquent brain tissue. The ability to achieve small, precise ablations—sometimes just a few millimeters wide—is vital. While larger ablations are often discussed, precision is equally essential for specific patient profiles where avoiding critical brain areas is paramount.
The software is particularly instrumental, offering a comprehensive, multi-slice view of the ablation area, which bo-osts the surgeon’s confidence in knowing exactly what is being targeted and, importantly, what is not.
The NeuroBlate System has always leveraged robotic control so that the surgeon, who conducts the procedure from the MR control room, can remotely move the laser probe to optimize their desired ablation zone. This cuts procedure time tremendously as the treating physician does not have to enter the MR room to make probe adjustments.
Robotics also optimizes laser probe placement within the lesion, allowing laser energy delivery that conforms to varying lesion shapes and sizes. Looking ahead, software updates will include faster data acquisition—cutting the time lag between MRI imaging and its integration into our system by nearly half. This is especially beneficial for targeting smaller ablation areas.
Additionally, we’re introducing enhancements for lar-ger ablations, such as adding more image slices per scan. This improvement means that instead of multiple scans with patient repositioning, a single scan will soon provide a complete view of the ablation target. These updates streamline the procedure and save valuable time.
What are Monteris’ goals and strategies for further innovation and collaboration within the neurosurgical community?
Emerson: Our company is built on the foundation of strong collaborative relationships with physician partners, including neurosurgeons, neuro-oncologists, medical oncologists, radiation oncologists, and epileptologists. This collaboration has been crucial in driving advancements across several areas including societal guidelines, market access, patient reimbursement, and educational programs in oncology and epilepsy.
From an R&D perspective, our collaboration with physicians directly influenced the development of the NB3 and has led to regular updates in our software and continued advancements in our products.
Additionally, our engagement with the medical community has facilitated significant clinical studies as mentioned. These efforts illustrate our deep commitment to integrating physician insights into our development process, which continues to fuel our innovation trajectory.
How does Monteris envision the future of neurosurgery with the continued development and integration of advanced technologies like the NB3 probe?
Emerson: Focusing on the oncology sector, our goal is to unite industry players, including physicians, pharmaceutical companies, and radiation therapy providers, to significantly enhance outcomes for patients with brain tumors. Given the grim reality of a glioblastoma diagnosis —which is almost invariably lethal —the current objective is to manage patient comfort du-ring their remaining days.
However, there’s growing excitement around innovative treatments, such as techniques to breach the blood-brain barrier, which could revolutionize therapy delivery, especially in terms of personalized medicine. Our technology plays a crucial role here; it facilitates opening the blood-brain barrier. This capability is pivotal for administering and activating personalized immunotherapies and other treatments, potentially extending patients’ lives while maintaining quality of life.
We are exploring how to leverage this in conjunction with other modalities like radiotherapy to enhance the therapeutic impact. This integration of advanced technologies and personalized treatment strategies represents future of oncological care, where our contributions could lead to significant advances in patient outcomes.
Could you provide some information about your professional journey and Monteris Medical?
Emerson: As a seasoned professional in medical technology, I've dedicated my career to this field, beginning with roles at notable companies like Baxter and Boston Scientific. My international experience includes significant stints in Singapore and Brussels, providing me with a broad perspective on product development and emerging technologies. My work has involved aiding companies in obtaining regulatory approvals and addressing issues related to reimbursement and patient access globally.
Over the past two decades, my career has been anchored in the Twin Cities. I served as CEO of American Medical Systems and later at Galil Medical, where we developed image-guided ablation technologies for various cancers, including bone, lung, kidney, prostate, and liver. Following the sale of Galil Medical to BTG, I transitioned to Monteris Medical due to shared investors and board members, leveraging my extensive experience in image-guided ablation.
Upon joining Monteris nearly eight years ago, I focused on enhancing a product that was effective but needed further validation and ease of use improvements. We aimed to expand our FDA label and strengthen reimbursement strategies. Having successfully addressed these areas, our recent efforts have concentrated on expanding our installed and procedural bases, ensuring that we continue to deliver and improve upon solid patient outcomes.











Comments
No Comments Yet!