The Impact of CAR-T Cell Therapies on the Future of Pediatric Cancer Care

ONCOLife |
24 May 2024
Dr. Robbie Majzner, a pediatric oncologist and independent investigator at Dana-Farber Cancer Institute, discusses the pivotal role of GD2 as a target in neuroblastoma and DIPG in this exclusive interview for ONCOLife. He highlights the dual action of FDA-approved antibodies that both mark cancer cells for immune destruction and block GD2’s immunosuperessive effects.
Despite the challenges of translating lab discoveries to bedside treatments and the high costs of trials, Dr. Robbie Majzner remains optimistic about harnessing T cells and CAR-T cell therapies to bridge the gap in treatment for rare pediatric cancers, underlining the importance of organizations like the V Foundation in supporting this vital research. His work not only aims to bring innovative therapies directly to children but also to inspire further advancements in the field.
Click the picture to view the PDF version: Pg 4-8.
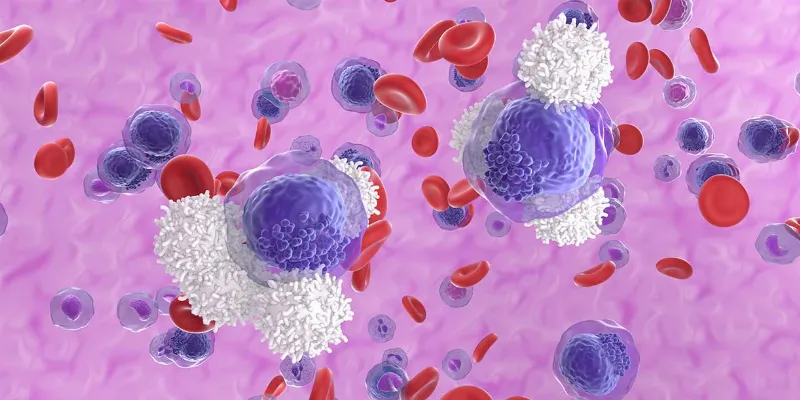
CAR-T cell therapies are poised to play a transformative role in pediatric cancer care, according to Dr. Majzner, setting a new standard in the efficacy and safety of cancer treatment. By targeting specific cancer markers like GD2, these therapies may represent a significant advancement in treating childhood cancers, including neuroblastoma and DIPG.
GD2: New Horizons in Cancer Immunotherapy
Could you explain how the expression of GD2 on DIPG cells contributes to the tumor’s aggressiveness and how targeting it with FDA-approved antibodies could revolutionize treatment?
Dr. Majzner: GD2, a molecule highly expressed on certain pediatric cancers, has been a key target in the fight against neuroblastoma, a cancer originating from developing nerve cells outside the brain. Since the 1980s, scientists have recognized the potential of GD2 as a target, and since the 1990s, two now FDA-approved antibodies targeting GD2 have significantly improved the survival rates for children with neuroblastoma. Despite this progress, the exact role of GD2 on cancer cells remained unclear until recent research revealed its immune-suppressive function.
My interest in immunotherapy and treating patients with neuroblastoma led my lab to investigate GD2 further. We discovered that GD2 suppresses the immune response against cancer, explaining its high expression levels on cancer cells. This discovery is pivotal, as GD2 is virtually absent on normal tissues, except during fetal development and at lower levels on brain and normal nerve cells in children.
With funding support from the V Foundation, Dr. Robbie Majzner is working to develop novel cellular immunotherapies for children with incurable cancers.
Essentially, cancer co-opts the protective mechanism of fetal development to evade the immune system. By targeting GD2 with immunotherapies, such as antibodies or CAR-T cells, we’re turning the tables on cancer, using its own mechanism against it. This strategy not only underscores neuroblastoma’s unique position as the only pediatric solid tumor with an effective FDA-approved immunotherapy but also serves as a blueprint for targeting other pediatric solid and brain tumors, highlighting the urgent need for innovative treatments in this area.
In my work, we have harnessed GD2-targeting immunotherapy to revolutionize how we approach pediatric cancers, notably neuroblastoma and DIPG, a universally fatal pediatric brain tumor. Despite advancements, about 50% of neuroblastoma patients relapse after receiving anti-GD2 antibodies, highlighting the need for more effective treatments. At Stanford, in collaboration with Michelle Monje’s lab, we discovered GD2’s high expression in DIPG.
Traditional therapies for DIPG are nearly non-existent, with most children succumbing within a year due to its inoperable nature. Our solution involved CAR-T cells engineered to cross the blood-brain barrier, a significant leap from the antibodies which couldn’t reach the brain. These engineered CAR
T cells can navigate the body to locate and attack DIPG cells directly in brain, showing promising early results in clinical trials.
New Research on CAR-T Cell Therapies
This journey of discovery and innovation underscores the potential of immunotherapy in treating pediatric cancers. By leveraging advanced immune engineering techniques, we’ve observed remarkable responses in DIPG patients, including cases with over 90% tumor shrinkage and even complete eradication lasting nearly two years. These outcomes were previously unimaginable for DIPG.
Having recently moved my lab to Dana Farber, I’m excited to continue this work, focusing on enhancing CAR-T cell efficacy through cutting-edge immune engineering. Our goal is to refine how these cells signal and interact within tumors, improving their ability to target and eliminate cancer cells while sparing healthy tissue.
This approach not only reaffirms the therapeutic promise of targeting GD2 but also sets a precedent for addressing other pediatric solid tumors and brain cancers, potentially transforming the treatment landscape for these devastating diseases.
The strategy to directly inject antibodies into the tumor represents a novel approach in the fight against DIPG. Can you share more about the preclinical results of this method, the timeline for potentially initiating clinical trials and any challenges you have faced?
Dr. Majzner: Originally, our project aimed to directly introduce treatments into the brain, a goal supported by our foundation grant. However, we’ve shifted our focus to utilizing CAR-T cells for GD2 targeting. These cells inherently navigate to their targets, eliminating the need for us to direct them manually.
This capability has significantly advanced our approach, allowing us to exploit the natural trafficking and im-mune surveillance abilities of CAR-T cells. They can autonomously locate and infiltrate tumors, even those within the brain, showcasing a remarkable breakthrough in cancer treatment.
How does your discovery that GD2 can suppress immune function open new avenues for immunotherapy, not just for pediatric cancers but potentially for other tumor types as well?
Dr. Majzner: It’s no coincidence that the only FDA-approved antibody in pediatrics targets GD2. This antibody not only flags neuroblastoma cells for immune removal but also inhibits GD2’s negative effects on immune health. By blocking the inhibitory signal GD2 provides, it enhances the therapy’s effectiveness. This dual-action approach—targeting cancer cells for destruction and lifting immune suppression—offers a potent strategy not just for pediatric cancers but for adult cancers as well, given GD2’s broad presence across various cancer types.
Dr. Majzner’s research emphasizes the potential of immunotherapy to transform treatment paradigms and offers new hope to children
We’re delving into the biology of GD2’s expression across different cancers, aiming to increase its expression on a wider array of tumors. This would allow us to employ this targeted strategy more broadly, leveraging the immune system’s full potential to combat cancer.
As a practicing pediatric oncologist, you are deeply involved in bringing early phase clinical trials of immunotherapies to children. What are the main obstacles in translating laboratory findings to bedside treatments, and how do you navigate these challenges?
Dr. Majzner: The journey from discovery to patient treatment is never quick enough, especially for those we see every day in our clinics. As researchers and clinicians, our drive often stems from our interactions with these patients, who face diseases we’re battling in the lab. This gap between discovery and application is a significant challenge; we’re constantly racing against time to develop new therapies for our patients.
The financial aspect of moving treatments from the lab to the clinic is daunting. Conducting a CAR-T cell clinical trial, for instance, can cost around $5 million, with limited grants specifically for such trials. While adult cancer treatments might find support in biotech and pharmaceutical sectors, pediatric cancer therapies rarely do. Historically, all three FDA-approved pediatric immunotherapies were advanced to clinical stages through academic efforts, highlighting the need for high-risk investment in rare diseases with costly development processes.
Moreover, the progression of GD2 CAR-T cell therapy illustrates the slow pace of clinical advancements. Since the mid-2000s, it’s taken about 20 years of iterative engineering and trials, occurring every 5 to 7 years, to develop effective treatments.
This slow process could be accelerated by more frequent trials and quicker learning from each iteration, but this requires funding models that support rapid iteration based on new learnings. Such funding would help speed up the cycle of trial analysis, grant writing, and the launch of new trials, especially crucial in pediatric oncology where developing a new therapeutic agent is both time-sensitive and expensive. This need for efficient funding mechanisms is critical to translating lab discoveries into life-saving treatments more swiftly.
Looking forward, what do you see as the most promising areas of research in pediatric oncology immunotherapy, and how does your work aim to address unmet needs in this field?
Dr. Majzner: Harnessing the power of T cells, the immune system’s most potent cancer-fighting entities, thro-ugh modern immune engineering, is the most promising area for attacking cancer cells, especially in pediatrics. The pharmaceutical industry often overlooks rare pediatric cancers due to their scarcity, but academia can develop, test, and potentially license these CAR-T cell therapies.
This approach offers pediatric oncologists a unique avenue to bring effective treatments directly to children, bypassing the lengthy process of waiting for therapies to adapt from adult treatments—which often fail to translate due to fundamental differences in disease biology.
Utilizing CAR-T cell engineering within an academic setting allows for rapid testing and development or the iterative re-engineering of treatments. This strategy aims to bridge the gap in treatment availability for rare pediatric cancers, providing a direct path from discovery to patient care without the commercial constraints faced by traditional pharmaceutical development.
What is the importance of organizations that fund cancer research like the work you are doing?
Dr. Majzner: Bridging pre- clinical research to clinical application is crucial, especially in pediatric oncology. The V Foundation plays a vital role in this process, providing essential funding where 100% is dedicated to developing new treatments for otherwise incurable diseases. This support is indispensable for advancing research and finding new therapies.
About Dr. Robbie Majzner
Dr. Robbie Majzner’s work in pediatric oncology aims to transform the treatment landscape for child-ren with incurable cancers through novel cellular immunotherapies, focusing on engineering safer and more effective CAR T cells, exploring the biology of GD2—a frequent pediatric cancer target, and launching early-phase clinical trials. His journey, inspired by witnessing the effects of CAR-T cell therapies during his NIH fellowship, reflects a shift from research disinterest to a passionate pursuit of innovative treatments for solid and brain tumors in children. Dr. Majzner’s program not only seeks to provide new therapeutic options but also to deepen the understanding of immune function suppression by cancer cells, leveraging this knowledge to advance therapeutic development and offer new hope in pediatric oncology.











Comments
No Comments Yet!