Engineered Immunotherapy Shows Promise in Cancer Treatments

ONCOLife |
25 November 2023
Researchers have developed a breakthrough cancer immunotherapy using engineered dendritic cell progenitors (DCPs) that do not require tumor antigen knowledge. The revolutionary technique, published in Nature Cancer, has the potential to significantly alter the landscape of cancer treatment. It offers a promising new direction in combating various forms of cancer.
In a groundbreaking study, scientists from the École Polytechnique Fédérale de Lausanne (EPFL), the University of Geneva (UNIGE), and the German Cancer Research Center have developed a new type of immunotherapy. Enhanced with IL-12 and FLT3L, these dendritic cell progenitors (DCPs) demonstrate remarkable effectiveness across various cancer models. They engage multiple immune components and synergize with CAR-T cells, offering potential for diverse cancer treatments.
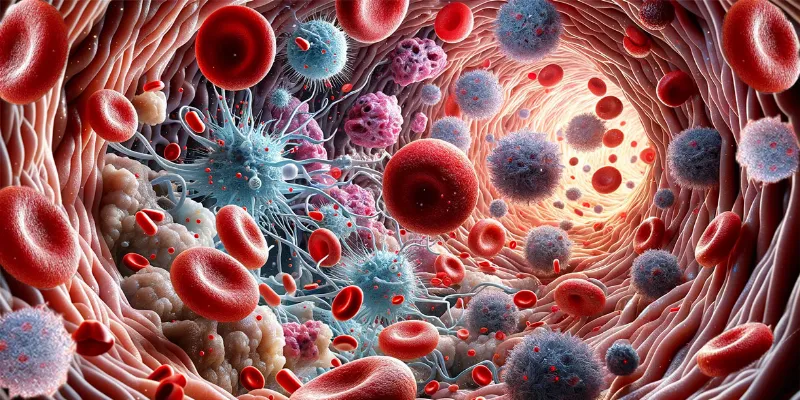
Understanding Dendritic Cells and Cancer
Dendritic cells are pivotal to our immune system. They capture and present antigens, including those from mutated cancer cells, to other immune cells, particularly the CD8 T cells, which play a critical role in eliminating infected or abnormal cells. However, tumors often evade this immune response by creating barriers that suppress the immune system, a process known as immunosuppression. This suppression includes inhibiting DCs from effectively presenting tumor antigens to CD8 T cells, allowing the cancer to grow unchecked.
Overcoming the Challenges of Traditional Vaccines
Traditional cancer immunotherapies, including DC vaccines, have aimed to counteract tumor-induced immunosuppression. These therapies typically involve creating DCs from a patient’s blood monocytes, exposing them to tumor antigens, and reintroducing them into the patient. Despite their potential, DC vaccines have yielded mixed results in clinical trials, partly due to their reliance on monocyte-derived DCs and predefined antigens, which may not represent the full spectrum of cancer cell antigens.
Engineered DC Progenitors
The research team, led by Michele De Palma, associate professor at EPFL and director of the Agora Cancer Research Center, has developed engineered DC progenitors (DCPs) capable of differentiating into type I conventional DCs (cDC1). These engineered DCPs stimulate anti-tumor immunity in mice, bypassing the need for the antigen-loading step. This significant advancement suggests a broader application against various human cancers, irrespective of the specific antigens they express.
“Our strategy does not use the monocyte-derived DCs employed in previous studies, but relies on a population of DC progenitors, called DCPs, which we can produce in vitro in the laboratory from readily available sources, such as blood and bone marrow,” said De Palma. He pointed out, “Remarkably, the engineered DCPs worked in the absence of antigen loading, which implies that they could be potentially effective against a broad range of human cancers, so irrespective of the antigens that they express. Our preclinical results require further development and testing before moving to clinical application”
Promising Preclinical Results
The engineered DCPs, armed with two immune-stimulatory molecules (IL-12 and FLT3L), have shown remarkable efficacy in various cancer models, outperforming traditional DC formulations. They have successfully unlocked the efficacy of CAR-T cells in eradicating brain tumors in mice, a particularly notable achievement given the limited success of CAR-T cells in brain cancer thus far. Professor Denis Migliorini, head of neuro-oncology at UNIGE, highlights the potential of combining DCPs with CAR-T cells in treating incurable brain cancer.
“A very promising result was the ability of the DCPs to unlock the efficacy of CAR-T cells in eradicating brain tumors in mice”, says Professor Denis Migliorini. He adds, “We are committed to combine DCPs with CAR-T cells in patients with incurable brain cancer.”
Towards Clinical Application
While these preclinical results are promising, further development and testing are needed before moving to clinical applications. The ability to readily obtain DCPs from human blood is a significant advantage in translating these preclinical findings into a transformative cancer immunotherapy.
Abstract of the research
Cytokine-armed dendritic cell progenitors for antigen-agnostic cancer immunotherapy
Abstract: Dendritic cells (DCs) are antigen-presenting myeloid cells that regulate T cell activation, trafficking and function. Monocyte-derived DCs pulsed with tumor antigens have been tested extensively for therapeutic vaccination in cancer, with mixed clinical results. Here, we present a cell-therapy platform based on mouse or human DC progenitors (DCPs) engineered to produce two immunostimulatory cytokines, IL-12 and FLT3L. Cytokine-armed DCPs differentiated into conventional type-I DCs (cDC1) and suppressed tumor growth, including melanoma and autochthonous liver models, without the need for antigen loading or myeloablative host conditioning. Tumor response involved synergy between IL-12 and FLT3L and was associated with natural killer and T cell infiltration and activation, M1-like macrophage programming and ischemic tumor necrosis. Antitumor immunity was dependent on endogenous cDC1 expansion and interferon-γ signaling but did not require CD8+ T cell cytotoxicity. Cytokine-armed DCPs synergized effectively with anti-GD2 chimeric-antigen receptor (CAR) T cells in eradicating intracranial gliomas in mice, illustrating their potential in combination therapies.










Comments
No Comments Yet!