Inverse Vaccine Could Treat Multiple Sclerosis and Autoimmune Diseases

New Discovery |
13 September 2023
Researchers have pioneered an 'inverse vaccine' capable of reversing autoimmune diseases like multiple sclerosis, type 1 diabetes, and Crohn's disease. This breakthrough doesn't suppress the overall immune system but strategically reduces its memory of specific molecules, preventing wrongful attacks on healthy cells.
Drawing inspiration from the liver's natural defense against autoimmunity, this innovative vaccine offers a promising, targeted treatment, already showcasing potential in Phase I trials for celiac disease.
Researchers at the University of Chicago's Pritzker School of Molecular Engineering have developed an "inverse vaccine" designed to treat autoimmune diseases. Unlike traditional vaccines that amplify immune responses, this vaccine diminishes the immune system's memory of specific molecules, preventing it from mistakenly attacking the body's healthy cells. This novel approach could offer more targeted treatment with fewer side effects.
Autoimmune diseases, including multiple sclerosis (MS), type 1 diabetes, Crohn’s disease, and rheumatoid arthritis, result from the immune system mistakenly targeting the body's healthy cells. Current treatments typically involve drugs that suppress the entire immune system, leaving patients susceptible to other illnesses and infections.
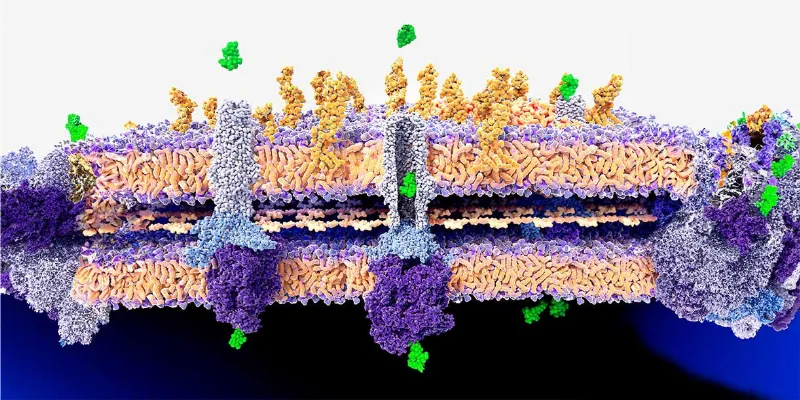
The "inverse vaccine" draws inspiration from the liver's inherent function of marking molecules from degrading cells with "do not attack" signals. By doing so, it prevents the body from erroneously targeting its cells. In this pioneering research, the PME team connected an antigen, which is the molecule that the immune system targets, with a molecule resembling a fragment of an old cell that the liver would recognize as benign.
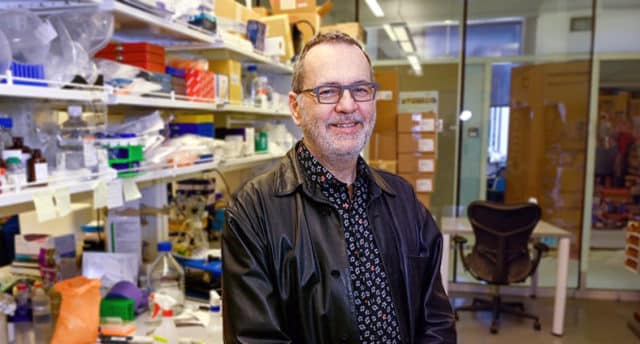
Jeffrey Hubbell, the Eugene Bell Professor in Tissue Engineering and lead author of the study, noted the significance of their findings, stating, “In the past, we showed that we could use this approach to prevent autoimmunit. But what is so exciting about this work is that we have shown that we can treat diseases like multiple sclerosis after there is already ongoing inflammation, which is more useful in a real-world context."
One of the pivotal elements of this research is the understanding and utilization of peripheral immune tolerance, a naturally occurring liver process. This ensures not every deteriorating cell in the body triggers an immune response. The researchers found that by tagging molecules with a specific sugar, N-acetylgalactosamine (pGal), they could replicate this tolerance mechanism.
Hubbell elucidated, "The idea is that we can attach any molecule we want to pGal, and it will teach the immune system to tolerate it.”
When the research team applied this method to an MS-like disease in animal models, they discovered that the immune system halted its assault on myelin, the protective sheath around nerves. This restoration of normal immune function reversed the symptoms of the disease.
Additionally, other experiments revealed the same technique effectively minimized ongoing immune reactions, suggesting a wide applicability across various autoimmune diseases. There's also been progress on the clinical front. Initial Phase I safety trials have been conducted on people with celiac disease, and further safety trials for MS patients are underway.
"There are no clinically approved inverse vaccines yet," Hubbell remarked, "but we're incredibly excited about advancing this groundbreaking technology."
Abstract of the research
Synthetically glycosylated antigens for the antigen-specific suppression of established immune responses
Abstract: Inducing antigen-specific tolerance during an established immune response typically requires non-specific immunosuppressive signalling molecules. Hence, standard treatments for autoimmunity trigger global immunosuppression. Here we show that established antigen-specific responses in effector T cells and memory T cells can be suppressed by a polymer glycosylated with N-acetylgalactosamine (pGal) and conjugated to the antigen via a self-immolative linker that allows for the dissociation of the antigen on endocytosis and its presentation in the immunoregulatory environment. We show that pGal–antigen therapy induces antigen-specific tolerance in a mouse model of experimental autoimmune encephalomyelitis (with programmed cell-death-1 and the co-inhibitory ligand CD276 driving the tolerogenic responses), as well as the suppression of antigen-specific responses to vaccination against a DNA-based simian immunodeficiency virus in non-human primates. Our findings show that pGal–antigen therapy invokes mechanisms of immune tolerance to resolve antigen-specific inflammatory T-cell responses and suggest that the therapy may be applicable across autoimmune diseases. For the full text of the article, click this link:>>> The reference for the article:>>>







Comments
No Comments Yet!