Immune Cell Diversity Could Revolutionize Flu Battle and Vaccine Strategies
18 November 2023
Scientists have discovered that specific immune cells present before flu infection can predict the likelihood of developing symptoms. This study challenges the traditional focus on antibodies for predicting flu susceptibility, highlighting the importance of a diverse set of immune cells, including T cells and natural killer cells, in providing protection.
Reserchers from St. Jude Children’s Research Hospital and the Institute of Environmental Science have unveiled new insights into predicting flu symptoms. Their research, recently published in Nature Immunology, shows that certain immune cells present before infection can more accurately predict the onset of flu symptoms than traditional methods.
Highlighting the critical role of diverse immune cells, including T cells and natural killer cells, the study opens new pathways for improving flu prediction and developing targeted treatments, revolutionizing our approach to flu prevention and care. The study not only offers new insights into flu prediction but also reinforces the importance of vaccination.
Understanding the Immune System’s Role
For years, the medical community has grappled with understanding why some individuals fall ill from infections while others do not. Richard Webby, Ph.D., from St. Jude’s Department of Host-Microbe Interactions, emphasizes that this study marks a significant advancement in resolving this mystery for influenza:
“We’ve been struggling for decades, with why some people get sick with infections and some don’t. This is one of the best attempts to try and figure that out for influenza. We were able to measure many different immune parameters from a single blood draw and correlate them with protection from, or susceptibility to, infection symptoms.”
Diverse Immune Cells: A Shield Against the Flu
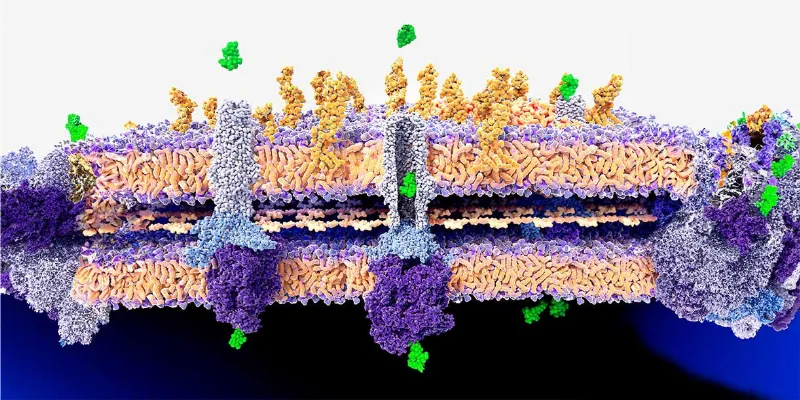
The research highlights that a functionally diverse set of immune cells correlates with increased protection against flu symptoms. By comparing blood samples of symptomatic and asymptomatic individuals, taken up to six months before the flu season, distinct differences were noted in their immune cell composition. Asymptomatic individuals exhibited a more varied set of immune cells, often associated with a long-term influenza-specific response, contrary to the more uniform inflammatory cells found in symptomatic patients.

Redefining Vaccination Strategies
The study leveraged data from the SHIVERS-II project, a community cohort-based surveillance in New Zealand, where volunteers regularly provided blood samples. The study suggests that focusing on promoting certain immune cell populations might be more effective than current approaches. Understanding the various immune profiles can help tailor vaccines to specific population needs, considering factors like age, sex, and previous infection history.
Senior researcher Paul Thomas, from St. Jude’s Department of Immunology, elaborates on how this research could reshape vaccination strategies:
“Our results show that the balance of different immune cells in people can be extremely biased. You might build up an immune cell army that is exceptional at fighting off one kind of infection, but then that can make you feel sicker from another kind of infection. By understanding which immune cells are the best for fighting the flu, we can start designing vaccines to push for those populations that are most protective.”
Predicting Flu Risk Beyond Antibodies
Traditionally, flu risk prediction has centered around the presence of anti-flu antibodies. However, this study reveals that considering a diverse set of immune cells, especially helper T cells, provides a more accurate prediction of protection. The researchers were able to make robust predictions about susceptibility to infection by combining cellular population data with serological antibody information.
“The baseline immune state before vaccination is known to significantly vary across age, sex, vaccination status, infection history and more,” said co-first author Aisha Souquette, Ph.D., St. Jude Department of Immunology. “By understanding the different types of immune profiles that can provide protective responses, we can tailor and optimize our vaccine platforms for populations with distinct baseline immune states.”
Implications for Public Health
The ability to predict who might be more likely to develop symptomatic influenza before the flu season even begins opens new avenues for public health interventions. This advance could lead to targeted support for at-risk individuals, improving our overall approach to flu prevention.
Abstract of the research
Baseline innate and T cell populations are correlates of protection against symptomatic influenza virus infection independent of serology
Abstract: Evidence suggests that innate and adaptive cellular responses mediate resistance to the influenza virus and confer protection after vaccination. However, few studies have resolved the contribution of cellular responses within the context of preexisting antibody titers. Here, we measured the peripheral immune profiles of 206 vaccinated or unvaccinated adults to determine how baseline variations in the cellular and humoral immune compartments contribute independently or synergistically to the risk of developing symptomatic influenza. Protection correlated with diverse and polyfunctional CD4+ and CD8+ T, circulating T follicular helper, T helper type 17, myeloid dendritic and CD16+ natural killer (NK) cell subsets. Conversely, increased susceptibility was predominantly attributed to nonspecific inflammatory populations, including γδ T cells and activated CD16− NK cells, as well as TNFα+ single-cytokine-producing CD8+ T cells. Multivariate and predictive modeling indicated that cellular subsets work synergistically with humoral immunity to confer protection, improve model performance over demographic and serologic factors alone and comprise the most important predictive covariates. Together, these results demonstrate that preinfection peripheral cell composition improves the prediction of symptomatic influenza susceptibility over vaccination, demographics or serology alone.








Comments
No Comments Yet!