AI Tool Shows Promising Results in Assessing Parkinson's Severity
16 September 2023
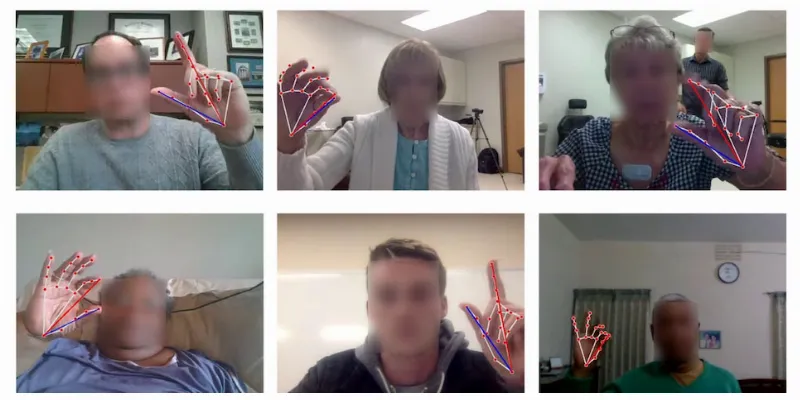
Researchers at the University of Rochester have developed an online artificial intelligence (AI), tool that allows individuals with Parkinson's disease to remotely and quickly assess symptom severity. Using a simple finger-tapping task captured by a webcam, the AI system, validated against medical professionals, provides swift evaluations. This pioneering development was detailed in a study recently published in NPJ Digital Medicine.
For the assessment, individuals are required to tap their fingers 10 times in view of a webcam. This seemingly straightforward motor task, commonly employed by physicians to gauge movement disorders, is then evaluated by the AI system on a scale of 0–4. The technology mirrors the benchmarks established by the Movement Disorder Society Unified Parkinson’s Disease Rating Scale.
What makes this AI model distinctive is its ability to instantaneously produce computational metrics such as speed, amplitude, frequency, and period—factors which, as per the research abstract, align remarkably with medical guidebooks and enable a precise categorization of tremor severity.

To validate the efficiency of this tool, a cohort of 250 international participants diagnosed with Parkinson’s disease underwent the finger-tapping task. The AI-generated evaluations were then juxtaposed with ratings by six medical professionals: three neurologists and three primary care physicians with UPDRS certification. Interestingly, while the AI lagged marginally behind expert neurologists, it surpassed the ratings by primary care physicians.
Reflecting on the broader implications, Ehsan Hoque, Associate Professor at Rochester Human-Computer Interaction Laboratory, stated:
“These findings could have huge implications for patients who have difficulty gaining access to neurologists, getting appointments, and traveling to the hospital. It’s an example of how AI is being gradually introduced into health care to serve people outside of the clinic and improve health equity and access.”
Moreover, the team believes their methodology is versatile, suggesting potential applicability in gauging other movement disorders, including ataxia and Huntington’s disease. Although the Parkinson’s assessment tool is accessible online, researchers advocate a judicious approach, cautioning against the sole reliance on this emergent technology devoid of physicians' insights for a conclusive disease diagnosis.
Abstract of the article
Using AI to measure Parkinson’s disease severity at home
We present an artificial intelligence (AI) system to remotely assess the motor performance of individuals with Parkinson’s disease (PD). In our study, 250 global participants performed a standardized motor task involving finger-tapping in front of a webcam. To establish the severity of Parkinsonian symptoms based on the finger-tapping task, three expert neurologists independently rated the recorded videos on a scale of 0–4, following the Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS). The inter-rater reliability was excellent, with an intra-class correlation coefficient (ICC) of 0.88. We developed computer algorithms to obtain objective measurements that align with the MDS-UPDRS guideline and are strongly correlated with the neurologists’ ratings. Our machine learning model trained on these measures outperformed two MDS-UPDRS certified raters, with a mean absolute error (MAE) of 0.58 points compared to the raters’ average MAE of 0.83 points. However, the model performed slightly worse than the expert neurologists (0.53 MAE). The methodology can be replicated for similar motor tasks, providing the possibility of evaluating individuals with PD and other movement disorders remotely, objectively, and in areas with limited access to neurological care.








Comments
No Comments Yet!