AI-Powered PET/CT Analysis May Predict Side Effects of Immunotherapy in Lung Cancer
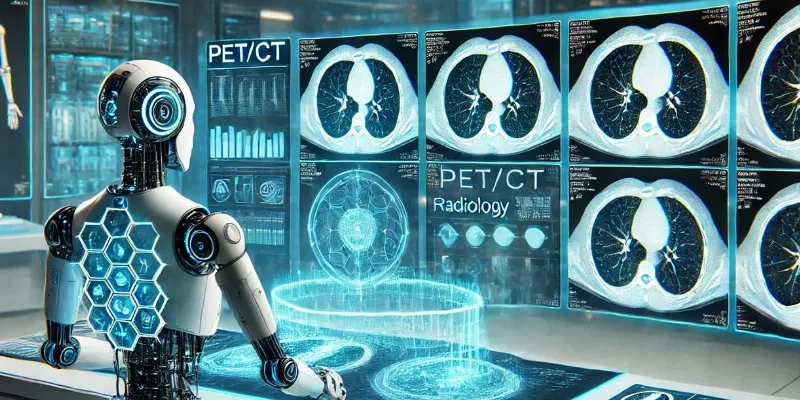
Artificial intelligence (AI) may help identify patients at risk of developing severe side effects from immune checkpoint inhibitors (ICIs) in lung cancer treatment, according to new research. The study, published in Academic Radiology, found that patients with high levels of inflammation in noncancerous lung tissue were 6.5 times more likely to develop interstitial lung disease (ILD), a potentially fatal complication of ICI therapy.
The study, conducted at Niigata University Medical and Dental Hospital in Japan, analyzed data from 165 lung cancer patients undergoing ICI therapy. Researchers led by Dr. Motohiko Yamazaki hypothesized that pre-existing inflammation in healthy lung tissue might increase the risk of ILD, a condition where immune cells inadvertently attack normal lung tissue.
Using AI, the team extracted and analyzed noncancerous lung regions from PET/CT scans taken within three months before ICI treatment. The degree of inflammation was quantified through specific metrics, including the maximum standardized uptake value (SUVmax) and total glycolytic activity (TGA).
The study revealed a stark difference in outcomes based on inflammation levels. Patients with high TGA values (≥149.45) had a 58.4% two-year cumulative incidence of ILD compared to just 14.4% in those with lower values.
Implications for Cancer Treatment
“PET/CT is generally performed to detect cancer metastasis, but it would potentially be useful for estimating the risks of side effects associated with cancer treatment,” said Dr. Yamazaki. “The results of our study may not only help to predict the occurrence of interstitial lung disease after immunotherapy, but also to elucidate the mechanism of this serious side effect.”
The study’s authors emphasize the need for further research. A multicenter prospective study could validate these findings and establish robust protocols for integrating inflammation metrics into clinical decision-making.
Understanding the Mechanism
Interstitial lung disease is believed to result from immune activation that damages healthy lung tissue alongside cancer cells. The researchers suggest that high inflammation in the lungs prior to therapy may predispose patients to this adverse reaction. By identifying at-risk individuals early, clinicians could tailor treatment strategies, potentially modifying or avoiding therapies likely to trigger ILD.
Expert Perspectives
The study represents a significant step toward precision oncology, where treatment decisions are guided by individual risk factors. With ICIs revolutionizing cancer care but posing severe risks for some patients, predictive tools like this could transform outcomes.
“We should conduct a multicenter prospective study for further investigation,” Dr. Yamazaki emphasized, pointing to the broader potential of AI-driven diagnostics.
The integration of AI into PET/CT imaging presents a promising avenue for mitigating risks in immunotherapy. By identifying patients likely to experience severe complications like ILD, healthcare providers can better personalize treatments, enhancing safety and efficacy.








Comments
No Comments Yet!